Estimated reading time: 11 minutes
Not long ago, I saw a 58-year-old man who had done “everything right.”
His LDL cholesterol (LDL-C) was well controlled on a statin, his blood pressure stable, and he exercised regularly. But he carried extra weight around his waist, his triglycerides were persistently high, and a CT scan revealed clear signs of atherosclerosis in his coronary arteries with a high coronary calcium score.
He was stunned. “But doctor, my cholesterol is fine. How can I still have heart disease?”
This question exposes a blind spot in modern cardiology. For decades, LDL-C — the so-called ‘bad cholesterol’ — has been the focus. And not without justification: evidence from large outcome trials confirms that lowering LDL translates into fewer heart attacks and strokes.
But LDL is not the whole story. In people with obesity, diabetes, fatty liver, or metabolic syndrome, another group of particles quietly fuels the fire: triglyceride-rich lipoproteins such as VLDL (very low-density lipoprotein) and their remnants.
These particles don’t just carry triglycerides. They carry cholesterol too — and often more cholesterol per particle than LDL itself. They slip into the arterial wall, get trapped, and set the stage for atherosclerosis. Today, research makes it clear: if we only look at LDL-C, we miss a big part of the disease.
This article is a rewriting and update of a piece I first published in 2017, reflecting the advances since then in our understanding of VLDL, remnant cholesterol, and their role in heart disease.
Lipid Couriers: What VLDL and Remnants Do
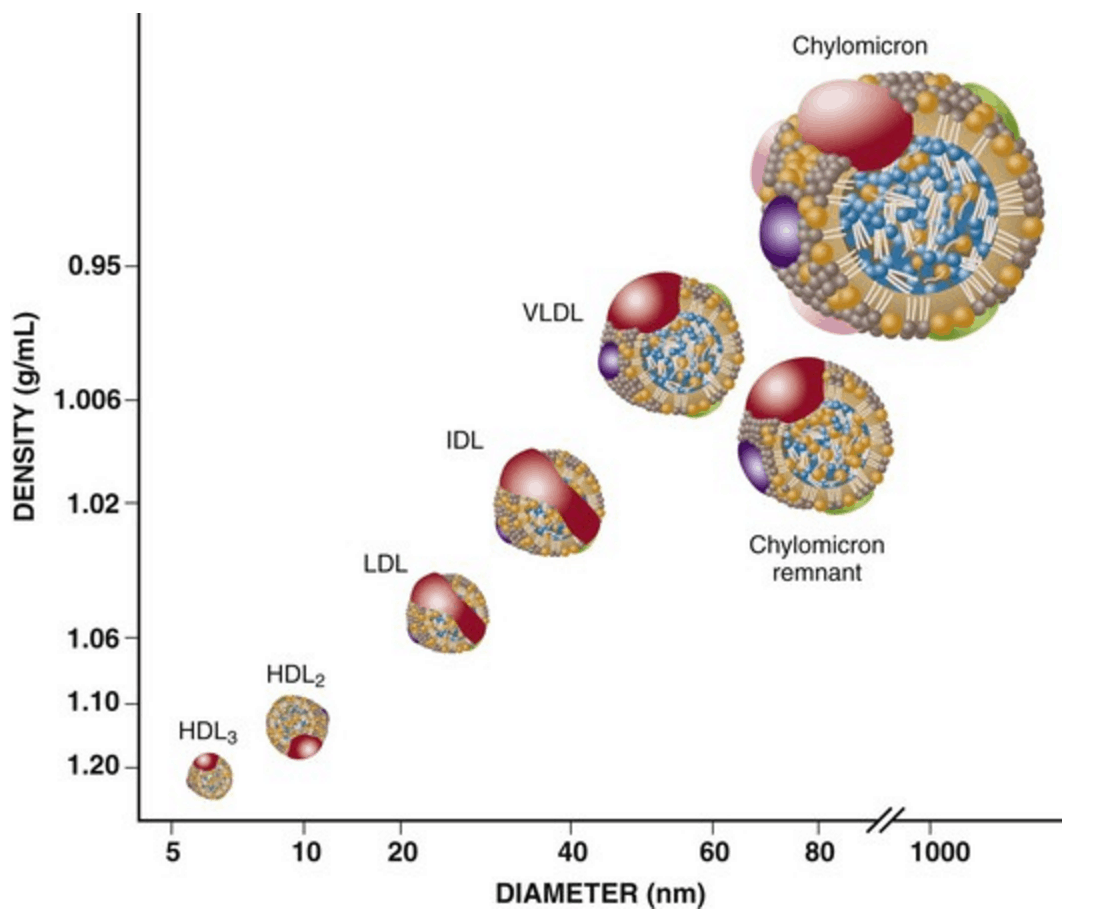
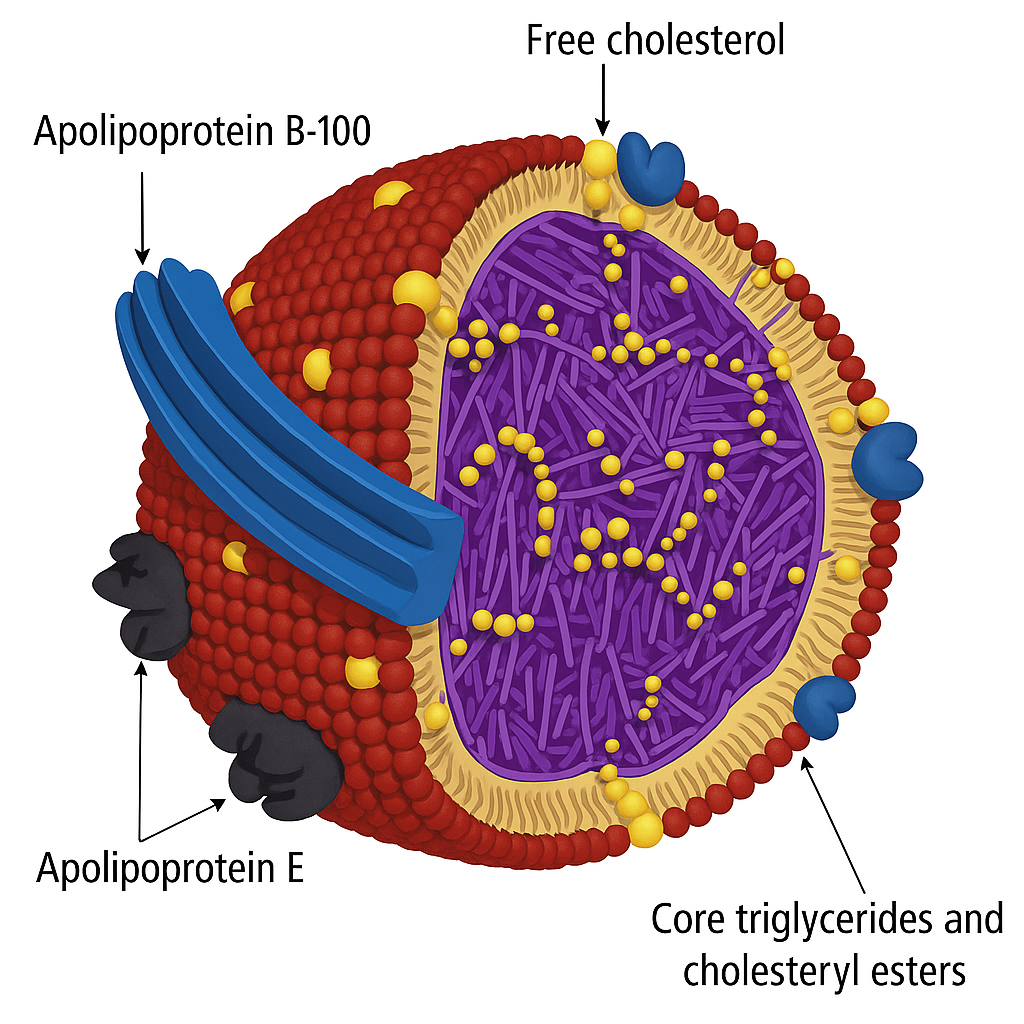
Lipoproteins are the body’s delivery trucks for fat. Because fat doesn’t dissolve in water, it can’t float freely in the bloodstream. Instead, it must be packaged into lipoproteins — tiny spheres with a shell of phospholipids and proteins and a cargo of triglycerides and cholesterol inside.
Most people have heard of LDL and HDL, but the larger, triglyceride-rich particles — chylomicrons and VLDL — are just as important.
-
Chylomicrons are made in the intestine after a fatty meal. They deliver dietary fat to tissues, then disappear within hours.
-
VLDL, made in the liver, circulates even in the fasting state. It transports triglycerides made from excess carbohydrate or fat, especially when insulin resistance drives fat flux from adipose tissue to the liver.
As VLDL particles unload triglycerides into tissues, they shrink and transform into remnants — smaller, cholesterol-enriched lipoproteins that linger in the bloodstream. These remnants are particularly dangerous because:
- They are small enough to penetrate the arterial wall.
- They carry far more cholesterol per particle than LDL.
- They are easily retained within the vessel wall, where they promote inflammation and plaque formation.
In short: LDL may be the “usual suspect,” but VLDL and its remnants are the stealthier, heavier-armed accomplices.
The Rise of VLDL in Modern Metabolic Disease
Half a century ago, fasting triglyceride levels weren’t a major concern in cardiology. The spotlight was almost entirely on LDL-C. But the world has changed.
We now live in an era of abundance and insulin resistance — an environment where VLDL production is cranked up day and night. Three forces drive this:
-
Obesity and visceral fat – excess fat tissue leaks fatty acids into the bloodstream, feeding the liver and pushing it to overproduce VLDL.
-
Carbohydrate excess – diets high in sugar and refined starches stimulate the liver to convert glucose into fatty acids (de novo lipogenesis), again packaged as VLDL.
-
Insulin resistance – the metabolic hallmark of type 2 diabetes and NAFLD, which blocks the normal brake on VLDL production.
The result: a bloodstream crowded with triglyceride-rich particles, many of which linger after meals instead of being cleared.
This pattern is more than a laboratory curiosity. It’s the metabolic fingerprint of the modern epidemic:
- Non-alcoholic fatty liver disease (NAFLD)
- Type 2 diabetes
- Hypertension
- The cluster we call metabolic syndrome
And with these conditions comes a heightened risk of premature atherosclerosis, even when LDL levels look deceptively “normal.”
In other words: the rise of VLDL is the rise of the chronic diseases that define our age.
Why Remnant Cholesterol Matters
If triglycerides are the fuel that VLDL carries, then remnant cholesterol is the hidden payload. And it’s this payload, not the triglycerides themselves, that makes remnants especially dangerous.
Remnant cholesterol is the cholesterol content of triglyceride-rich lipoproteins — VLDL, IDL, and chylomicron remnants. Once these particles have shed some of their triglycerides, what remains is a smaller, denser, cholesterol-enriched lipoprotein that lingers in the bloodstream.
Why does this matter?
-
They carry more cholesterol per particle than LDL. Each remnant can deliver five to twenty times the cholesterol of a typical LDL particle.
-
They penetrate the artery wall easily. Their size and composition allow them to slip past the endothelium and get trapped in the subendothelial space.
-
They trigger inflammation. Once retained, they promote oxidative stress, foam cell formation, and plaque buildup.
Over the past decade, the evidence has hardened. Large genetic studies show that elevated remnant cholesterol is a causal factor in atherosclerotic cardiovascular disease, independent of LDL. Mendelian randomization analyses confirm the direction: more remnants, more risk.
In fact, one landmark analysis found that a 1 mmol/L (about 39 mg/dL) increase in nonfasting remnant cholesterol was associated with nearly a threefold higher risk of coronary heart disease.
This explains why patients with metabolic syndrome often get heart disease even when their LDL looks “fine.” Their bloodstream is filled with cholesterol-rich remnants that quietly do the damage.
Measuring the Invisible
If remnants are so dangerous, why don’t we routinely measure them in the clinic? The short answer: it’s not easy. Unlike LDL-C, which has been standardized for decades, there’s no simple blood test labeled “remnant cholesterol.”
But there are practical ways to get at it:
Non-HDL cholesterol
- Calculated as total cholesterol – HDL cholesterol.
- Captures the amount of cholesterol in ApoB-containing particles: LDL + VLDL + IDL + remnants.
- Free, universally available, and consistently a better predictor of risk than LDL-C alone.
ApoB
- A direct count of particle number — one ApoB per particle, whether LDL or VLDL.
- More precise than LDL-C, especially when triglycerides are elevated.
- Increasingly recommended by international guidelines, though still underused in practice.
Remnant cholesterol (calculated)
- Can be estimated as total cholesterol – LDL-C – HDL-C.
- Used in research settings and sometimes in clinics, but not yet a standard part of risk assessment.
The lesson is simple: LDL-C alone is not enough. In a world where obesity, diabetes, and fatty liver are common, measuring particle burden (ApoB) or total atherogenic cholesterol load (non-HDL-C) gives a far clearer picture.
This shift is already making its way into guidelines. The European Society of Cardiology now recommends non-HDL-C and ApoB as secondary treatment targets. The American guidelines are catching up too. Slowly, the message is spreading: to prevent heart disease, you need to count all the atherogenic particles, not just the LDL fraction.
VLDL is produced by the liver. It carries both cholesterol and triglycerides.
How to Lower VLDL and Remnants
The good news is that VLDL and remnants are not untouchable. They respond to lifestyle, and we now have therapies that specifically target them.
1. Lifestyle first
-
Weight loss: Even a 5–10% reduction in body weight can meaningfully lower triglycerides and VLDL production.
-
Exercise: Regular physical activity increases muscle uptake of triglycerides and improves insulin sensitivity.
-
Cutting sugar and refined carbs: Added sugar, high-glycemic starches, and especially fructose drive fatty acid synthesis in the liver and boost VLDL output.
-
Moderation with alcohol: Even modest drinking can raise triglycerides, and heavy use may cause dangerous spikes.
-
Managing insulin resistance: Addressing type 2 diabetes, prediabetes, or fatty liver disease helps take the liver’s VLDL factory off overdrive.
2. Medications
-
Statins: They remain the backbone of therapy, reducing ApoB particle numbers across the board. They do lower triglycerides somewhat, though not as powerfully as LDL.
-
Omega-3 fatty acids: High-dose prescription EPA (icosapent ethyl) showed a 25% reduction in cardiovascular events in the REDUCE-IT trial (2018). But not all fish oil products are equal — mixed EPA/DHA trials (like STRENGTH) did not replicate the same benefit.
-
Fibrates: Once popular for triglyceride lowering, they show mixed results on outcomes, but may still be useful in selected patients with high triglycerides and low HDL.
-
New therapies on the horizon:
-
ApoC-III inhibitors (like olezarsen) and ANGPTL3 inhibitors (like evinacumab) slash triglycerides and remnant particles by targeting the proteins that regulate lipoprotein metabolism.
-
These are still emerging, but they signal a future where we can treat high-remnant states with precision.
-
3. Special situations
In patients with very high triglycerides (above 500–1000 mg/dL), the priority shifts: preventing pancreatitis. Here, strict reduction of dietary fat and alcohol is critical, along with medications if needed.
The Future of Lipid Management
For decades, cholesterol management has meant one thing: lower LDL-C. That strategy remains important, though newer evidence shows it doesn’t capture the whole picture. The focus is shifting to ApoB particle number overall, with growing recognition that triglyceride-rich remnants deliver a disproportionately large cholesterol load — and therefore risk — per particle.
Three shifts are already underway:
1. From LDL-C to ApoB and non-HDL-C
-
LDL-C remains useful, but it’s an incomplete marker.
-
Non-HDL-C and ApoB capture the entire family of atherogenic particles — LDL, VLDL, IDL, and remnants.
-
Expect guidelines and clinicians to lean more heavily on these markers, especially in patients with metabolic syndrome or diabetes.
2. From fasting to postprandial thinking
-
Most of our day is spent in a “post-meal” state, when triglyceride-rich lipoproteins peak.
-
Remnants generated in this state may be more relevant to plaque growth than fasting LDL.
-
Future risk assessment may focus more on postprandial lipids and remnant burden.
3. From broad strokes to precision therapies
-
Statins and ezetimibe remain cornerstones, but we are moving into a new era.
-
Icosapent ethyl (EPA-only omega-3) already showed that targeting triglyceride-rich lipoproteins can reduce events.
-
In development: ApoC-III and ANGPTL3 inhibitors, which dramatically cut triglycerides and remnants, potentially transforming care for patients with stubborn hypertriglyceridemia.
Conclusion – Beyond LDL
The man I saw that morning went home with a new understanding. His LDL cholesterol was “fine,” but his triglycerides, his waistline, and his fatty liver were all telling the same story: his bloodstream was crowded with VLDL and remnants, and those particles were silently delivering cholesterol into his arteries.
For him, the answer wasn’t just another LDL check. It was weight loss, cutting back on refined carbs and alcohol, more exercise, and yes, staying on his statin. But most importantly, it was shifting the focus from a single lab number to the bigger picture of ApoB particles and remnant cholesterol.
LDL reduction remains vital, but in the era of metabolic disease, it’s not enough. To truly prevent heart disease, we have to look beyond LDL — at the triglyceride-rich particles that carry hidden cargo and fuel tomorrow’s plaques.
Related Reading on Doc’s Opinion
- The 12-Step Biology of Atherosclerosis (link)
- Non-HDL Cholesterol: The Hidden Heart-Disease Predictor You’ve Overlooked (link)
- Atherogenic Dyslipidemia (link)
- When High LDL Leads to Heart Disease — And When It Doesn’t (link)
- The Triglyceride/HDL Cholesterol Ratio (link)
- LDL-C vs. LDL-P: What’s the Difference? (link)
- What’s the Best Lipid Marker to Predict Risk? (link)
- High Triglycerides — And How to Lower Them (link)
- Apolipoprotein B (ApoB) and the Real Risk of Heart Disease (link)
- HDL Cholesterol — The Good, the Misunderstood (link)
- 10 Pitfalls of Using LDL-C to Assess Risk (link)
- The Role of Low-Density Lipoprotein (LDL) in Atherosclerosis and Heart Disease (link)
- LDL Particle Number vs. Size — Made Easy (link)
- LDL-P (link)
- Lipoprotein(a): The Overlooked Particle That Most Cholesterol Tests Miss (link
References
- Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. Eur Heart J. 2017;38(32):2459-72.
- Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626-35.
- Varbo A, Benn M, Tybjærg-Hansen A, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61(4):427-36.
- Varbo A, Benn M, Nordestgaard BG. Remnant cholesterol as a cause of ischemic heart disease: evidence, definition, measurement, atherogenicity, high risk patients, and present and future treatment. Pharmacol Ther. 2014 Mar;141(3):358-67. doi: 10.1016/j.pharmthera.2013.11.008. Epub 2013 Nov 26. PMID: 24287311.
- Jørgensen AB, Frikke-Schmidt R, West AS, Grande P, Nordestgaard BG, Tybjærg-Hansen A. Genetically elevated non-fasting triglycerides and calculated remnant cholesterol as causal risk factors for myocardial infarction. Eur Heart J. 2013 Jun;34(24):1826-33. doi: 10.1093/eurheartj/ehs431. Epub 2012 Dec 17. PMID: 23248205.
- Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11-22. (REDUCE-IT trial)
- Nicholls SJ, Lincoff AM, Garcia M, et al. Effect of high-dose omega-3 fatty acids vs corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH Randomized Clinical Trial. JAMA. 2020;324(22):2268-80.
- Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (FIELD study): randomised controlled trial. Lancet. 2005;366(9500):1849-61.
- Ballantyne CM, Braeckman RA, Soni PN, et al. Efficacy and safety of volanesorsen in patients with hypertriglyceridemia: a randomized clinical trial. Nat Med. 2016;22(5):492-501.
- Graham MJ, Lee RG, Bell TA, et al. Antisense oligonucleotide inhibition of apolipoprotein C-III reduces plasma triglycerides in rodents, nonhuman primates, and humans. Circ Res. 2013;112(11):1479-90.


Doesn’t high-dose niacin (the immediate-release form, in doses of 2 grams or more per day) also effectively reduce triglycerides?
Yes it does. Good point Barry.
Niacin at doses of 1500 to 2000 mg daily can reduce triglyceride levels by 15 to 25 percent
I did leave out drug therapy here but have dealt with it in another blog post
https://www.docsopinion.com/2016/01/03/high-triglycerides-lower-triglycerides/
Thanks, Doc!
My friend wrote the foreword to Niacin: The Real Story so he has me on the bandwagon. I take 4 grams a day, eat low low carb with lots of meat & fat, & have since 2018. My remnant particles are 17mg/dL, have good ApoB, and Lp-a, and have never felt better since I’ve been alive. I started taking niacin in 2021 when I read the book during the pandemic. I love your work & your articles, and just enjoyed listening to your Sunday Blues story!! Thanks for sharing & being so thoughtful.
Thank you so much Briana for sharing this — and for the kind words about my work. I’m glad the Sunday Blues story resonated with you. It sounds like you’ve found a path that really works for you, both in how you feel and in your lipid profile. Niacin is such an interesting chapter in the story of cardiovascular prevention — controversial, sometimes overlooked, but with a long history. I always enjoy hearing how people integrate these ideas into their own lives. Grateful to have you reading and listening.
I live in Cleveland Ohio in the U.S. (where the famed Cleveland Clinic is located) and would like to find a clone of you here. : ) Meaning, I wish I had a doctor I could go see, to go over my cholesterol issues. Would you happen to be able to suggest one? I continue to have high cholesterol and am exercise, eat very well, am not overweight, etc. and my doctor wants me to start meds and I don’t want to. So I’d like to go over my numbers with someone and see if something might be done besides medication (I can’t swallow fish oil capsules) Thanks for all your wonderful articles.
A well researched and written article on a very complex topic. Much appreciated.
Dr Sigurdsson,
I take Ezetimibe for the ApoB and I switched my statin to pitavastatin some time ago. Is pitavastain any better than the older statins on this VLDL and remnant category? I searched your website for pitavastatin but nothing came up.
The mornings are getting dark here in PA, I can’t imagine what Iceland is like in the mornings.
Phil
Phil, pitavastatin’s a good choice—especially with its neutral effect on glucose—but in terms of ApoB and remnants it performs much like the older statins. Ezetimibe is a smart add-on when remnants or triglycerides linger. The mornings are still bright here in the North Atlantic, but there’s no mistaking that autumn is on its way.
Thank you for getting back to me about the pitavastatin. I take the 1mg pitavastain and the 10 mg ezetimibe. My Lp(a) tested fine (21 nmol/L) so this seemed like the best combination presently available. I’ll stay tuned to your channel to see what is coming but I think at 77 years old this is it for me.
After I wrote my day-length comment yesterday I realized that your day-length is still much longer that ours.
In the 60’s and I lived in Annapolis MD I dated an 18 year old whose mother was from Iceland (at that time the father was gone). I wish I could remember her name you might have known the family. I was a Vietnam War rebel and was going to move back to Iceland with the daughter! Obviously I never made it!
Thanks for all you do.
Phil
Phil, thank you for sharing this. Your combination of low-dose pitavastatin with ezetimibe makes good sense — especially with your ApoB and Lp(a) numbers looking favorable. At 77, that’s a solid place to be, and I agree it’s often less about chasing “more” therapy than staying steady with what works.
I also enjoyed your Annapolis story — Iceland does have a way of weaving itself into unexpected corners of people’s lives! Thank you for following along here, and for your kind words.