Estimated reading time: 5 minutes
A recently published scientific paper shows that measuring cholesterol levels in the blood may not be an optimal tool to predict the risk of cardiovascular events (1). The study is especially important because our confidence in cholesterol, LDL-cholesterol (LDL-C) in particular, has been pretty consistent for a very long time.
The paper, published by Marston and coworkers, underlines the importance of lipoproteins containing apolipoprotein B (apoB) and their key role in the development of atherosclerotic heart disease. The study shows that the risk of myocardial infarction (heart attack) is best captured by the number of apoB-containing particles, independent of their cholesterol or triglyceride content.
Surely, we have known for decades that there is an association between circulating levels of cholesterol and cardiovascular risk. Numerous studies have shown a strong correlation between LDL-C and the risk of coronary heart disease (2,3,4,5). Moreover, cholesterol-lowering drugs have been shown to improve cardiovascular health (6).
So, we have come to believe that we should always aim at lowering LDL-C, whether it be by dietary measures or by drug treatment (7). Our progress, or lack thereof, could then be simply tested by checking the cholesterol numbers.
However, as I have pointed out in several blog posts over the years, relying on LDL-C to predict cardiovascular risk has many pitfalls (7,8,9).
Unfortunately, the deep-rooted and oversimplified cholesterol model of heart disease often leads us off-target and frequently promotes erroneous conclusions. Therefore, the study by Marston and coworkers is of huge importance.
Apolipoprotein B and Cholesterol – The Carrier and the Cargo
Cholesterol is an essential substance for the human body. Our liver constantly generates cholesterol. It is believed that only about 20 percent of the cholesterol in our bloodstream comes from the food we eat, the rest is produced by the liver. (10).
To be able to get to cells and organs, cholesterol has to be transported in the circulation. However, since cholesterol is a fat, it can’t travel in the bloodstream by itself,
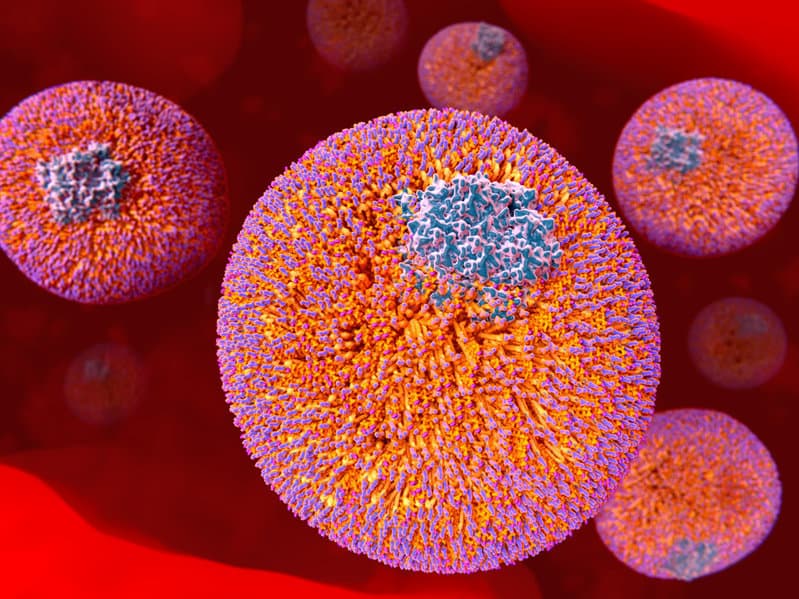
The body solves the problem by packaging cholesterol together with proteins (apolipoproteins) that function as carriers, transporting important cholesterol molecules to the cells of the body. These combinations of fats and protein are termed lipoproteins.
The apolipoproteins are the carriers whereas the cholesterol is the cargo.
Different lipoproteins contain different types of apolipoproteins. The type of apolipoprotein present determines the structure and function of the lipoprotein.
There are several classes of apolipoproteins and many subclasses (11).
The amount (mass) of cholesterol in each lipoprotein particle is variable. For example, some LDL particles carry small amounts of cholesterol whereas other particles carry large amounts. Hence, the difference between small and large particles.
Atherogenic Lipoprotein Particles
There are six major types of lipoproteins; chylomicrons, very-low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and Lipoprotein (a).
Evidence shows that lipoproteins play a fundamental role in atherosclerosis.
Some lipoproteins tend to interact with the arterial wall and initiate the cascade of events that leads to atherosclerosis which may progress to atherosclerotic cardiovascular disease (8). These lipoproteins are termed atherogenic.
The presence of apoB determines whether an apolipoprotein is atherogenic or not. Atherosclerosis is only promoted by aboB containing lipoprotein particles.
Trapping of apoB-containing lipoprotein particles within the arterial is a primary cause of atherosclerosis.
The mass of cholesterol within the lipoprotein particle does not influence whether it gets trapped within the arterial wall or not. Thus, the lipoprotein’s atherogenicity is determined by the surface protein, not the cholesterol.
Atherogenic lipoproteins such as LDL, VLDL, and Lp(a), all contain one ApoB100 molecule per particle.
Thus, all atherogenic lipoprotein particles contain one ApoB molecule each. Ergo, we can count the number of atherogenic particles by counting the number of ApoB molecules.

LDL-C, Non-HDL-C or ApoB
A standard serum lipid profile measures the concentration of total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. The LDL-C concentration is usually estimated from these numbers by using the Friedewald equation.
Over the years, LDL cholesterol (LDL-C) has been the most commonly used lipid variable to predict cardiovascular risk (12). However, recent evidence suggests that non-HDL cholesterol (non-HDL-C) may be a better tool for risk assessment (13,14).
Non-HDL-C is calculated by subtracting HDL-C from the total cholesterol. Hence it provides a measure of the amount of cholesterol carried by all lipoproteins except HDL.
Non-HDL-C will give us the amount of cholesterol carried within all atherogenic lipoproteins. In other words, a measure of cholesterol carried by all the “bad” lipoproteins but not the “good” ones (which is only HDL).
Importantly, LDL-C and non-HDL-C do not tell us anything about the number of atherogenic particles. They only provide information about the mass of cholesterol carried by the different types of lipoproteins.
Due to the fact that the mass of cholesterol per particle is variable, LDL-C and non-HDL-C can differ significantly from apoB.
In their recent study, Marston and coworkers provide evidence from a large prospective observational study (the UK biobank) and two large clinical trials (FOURIER and IMPROVE-IT) that cardiovascular risk is best predicted by measurements of apoB.
The study also shows that LDL-C and non-HDL-C are nonsignificant markers of risk when apoB is taken into account.
When cholesterol-depleted particles are present, LDL-C and non-HDL-C will underestimate risk. Conversely, when cholesterol-rich particles are present, LDL-C and non-HDL-C will overestimate risk.
So, it appears that LDL-C and non-HDL-C are unreliable surrogate markers of the number of atherogenic lipoprotein particles. ApoB on the other hand provides a reliable measure of particle number and is currently the best available lipid marker to predict cardiovascular risk.
Interestingly, apoB can be measured inexpensively, and more accurately than LDL-C or non-HDL-C by currently available methods (15).
Why not end the dispute? From now on, measurements of apoB should be used when deciding whom to target and how aggressively to treat people at risk and patients who already have established cardiovascular disease.

Agree ApoB should be measurement of choice Hope LPa will gain prominence as an important risk factor as huge potential if anti-sense oligonucleotide phase 3 trial proves successful
Hi Andrew
Agree. It will be interesting to learn nore about the clinical efficacy of Lp(a) specific lowering medications.
I tried, unsuccessfully, to get into the HORIZON study, but was refused, due to the fact that I haven’t experienced a MACE. But…I’m 66, my father was 42 when he was suddenly taken by an MI, my one-year older brother had a 4x bypass ten years ago, my lp(a) is 345, my calcium scan result is 1210, and I had a TIA at work some time ago. I’m instructing my wife to take my dead body and leave in the lobby when I keel over, maybe that can get some useful information from my corpse!
Would this insight make any difference in finding new treatment targets? Would bind/inactivate only apoB bound cholesterol be feasible?
Absolutely Robert.
Knockdown of ApoB by antisense oligonucleotides is currently being studied. Mipomersen, a sequence-specific antisense oligonucleotide targeting ApoB mRNA is presently being tested in clinical trials.
Doc, I just sent a reply to Andrew. I’ve been researching CVD and the pathogenesis of atherosclerosis intensively for some years. I myself have significant CVD, calcium score=1210, lp(a)=345,plaque in my carotids, etc. I just want to commend you on your putting this information out there in a plain and useful manner. It’s been so frustrating dealing with the whole cholesterol smoke-screen for the last 55+ years, knowing that there is so much that they don’t know, yet my very life depends on the truth! Anyway, thanks so much for guys like you!
Very well written and instructive article, Axel.
Always a pleasure to read you and to learn from you.
Thanks for sharing your knowledge.
😊
Thanks Jude.
Appreciate your interest 🙂
Nice to get better information about what’s going on in our arteries…..I had a heart attack in 2009, a stent was put in my left descending artery,and since then I’ve tried to be my own best friend and learn and understand what I have to do to improve my heart health . Thanks for this good information.
Thanks for sharing your thoughts Shaun.
Wish you all the best 🙂
A great article that I have been waiting for a very long time, as it has been talked about since 2015. Thank you
Very insightful and timely article. I just received my CardioIQ results and ApoB is 79 mg/dL (apparently optimal is < 90) and Lp(a) is 102 nmol/L (moderate risk category is 75 – 125). Not sure how to interpret since one is good, the other one not so much. Most importantly, how do I convince my primary care physician that ApoB is more important to pay attention to than LDL?
Thanks,
D
Super! Thank you Dr Sigurdsson. I have a cardiology appt coming up soon. Should I ask to have ApoB and Lp(a) tested?
I am a retired 69 year old dentist in the US. My education had both dental and medical students training together for the first two years in addition to my doing a hospital based residency. As a result I have had an interest in understanding the etiology of this disease and its detection. It seems there is a lacking when it comes to testing for early detection before the disease has taken a foothold later in life.
I am very interested in educating myself more on CVD/ lipoproteins and wonder if you could recommend a source(s) for an up to date summary on the etiology of atherosclerosis ?
Hi Chuck
Take a look at this article. It might be a good start:
https://www.docsopinion.com/low-density-lipoprotein-atherosclerosis-heart-disease/
Readers,
More on apoB here: https://peterattiamd.com/allansniderman/ I’m not sure how much of this interview is available without a (paid) subscription.
Dr. Sigurdsson,
I have been low carb for 20 years and will get my apoB tested with my next bloodwork per your reccommendation and others.
Other than following a low carb life style what else is available to lower one’s apoB number?
Philip Thackray
Very interesting article. How does the TG/HDL Ratio compare to the apoB measurement as a predictor of the risk of heart disease?
An interesting recent article on the TG/HDL Ratio:
Triglycerides and low HDL cholesterol predict coronary heart disease risk in patients with stable angina (October, 2021)
https://www.nature.com/articles/s41598-021-00020-3
Hi Jeffrey
Thanks for sharing this paper.
Interestingly, the study shows that the TG/HDL-C ratio was weakly related with LDL-C but strongly and positively related with Apo B .
The TG/HDL-C ratio may indeed reflect particle number? We know that a high TG/HDL-C ratio indicates a preponderance of small particles. A small particle carries less cholesterol than a large particle. Therefore, a greater number of particles is needed to carry a certain amount of cholesterol if the particles are small than if they’re large. So, a high TG/HDL-C ratio likely reflects a large number of LDL-particles and would then logically correlate with ApoB.
https://www.docsopinion.com/triglyceride-hdl-ratio/
Thanks Phillip
Very good. I was not aware of this interview.
Of course Dr. Sniderman is THE expert when it comes to ApoB.
Dr. Sigurdsson,
Perhaps you are aware of Dr. Sniderman’s ApoB “app”?
See here: https://apob.app/
The app requires entering your ApoB, your triglycerides and your total cholesterol. numbers.
I too listened to the full Peter Attia podcast with Dr. Sniderman. The podcast should be shared with all our docs as should your excellent article.
Thank you! When will we all wake up and why can’t we practice preventative medicine in this country?
Curious if you have read Malcolm Kendricks latest book “The Clot Thickens?” and your thoughts on that? https://drmalcolmkendrick.org
Thanks,
Mark
Hi Mark
I haven’t read Dr. Kendirck’s book.
Somewhere I think the comment I left got lost so thought I’d post again. Sorry if it gets duplicated! I was recently reading Dr Malcolm Kendrick’s “The Clot Thickens” and was wondering what your take was on it, since he dismisses LDL as the major cause of plagues. Curious
How is it possible that Lipoprotein (a) is bad when there are many articles on Pubmed about Centenarians that have elevated levels of Lp(a) which are in the genetics for a good reason as to be protective and keep a person in good health for over 100 years? Please explain.
What articles are you referring to?
https://pubmed.ncbi.nlm.nih.gov/9535215/
https://pubmed.ncbi.nlm.nih.gov/9622284/
https://pubmed.ncbi.nlm.nih.gov/9543111/
https://link.springer.com/article/10.2165/00044011-199611040-00007
https://pubmed.ncbi.nlm.nih.gov/11890580/
Hi there. I received some worrying results last week.
I am female, aged 40. I have been in fertility treatment for 2yrs. Diagnosis is Diminished Ovarian Reserve, essentially peri menopausal since I was 37 (possibly earlier). Severely low oestrogen and very high FSH. Each round of IVF is approx 3 weeks of birth control and up to 6mg per day of Estrace. I’ve had optimum cholesterol levels every year until this year in March when they were mildly elevated. My blood pressure has always been optimal and still is. I started to experience shortage of breath when breathing out this august. I had an echocardiogram which came back all normal.
A couple of weeks ago I went and had a lot of bloodwork and today received;
LDL-P 2156
LDL- C 134
HDL- C 54
Triglycerides 149
Total Cholesterol 202 or 214 (two readings)
Small LDL-P 1137
LP-IR Score 67
Omega Check 4.3
LDL Chol Calc (NIH) 128
C-Reactive Protein, Cardiac 5.74
HDL-P (total) 41.4
LDL size 20.6nm
Dads health is unknown. My moms family have a history of diabetes type 2 & my mom had two stents aged 66 with no prior cardiac issues. Her father died of a massive heart attack.
5ft 5in, 175lbs (should be 140lbs), no past health issues except suffer quite bad cold sores.
To add it turned out I had covid when these results were drawn & suffered tight chest and shortness of breath. I’m now concerned that this was reflective of these results v covid.
My doctor emailed these results with zero follow up. I’ve tried to call him multiple times with no success.
Is this something I should worry about?
I’m not a doc, but if I were you I would boost my Omega-3 intake.
I assume that Omega Check refers to the Omega-3 index. Boosting your Omega-3 intake would increase your Omega-3 index and lower your TG/HDL-C ratio. My Omega-3 index is 9.4% and my TG/HDL Ratio is 1.5. I take about 3,000 mg per day of EPA + DHA.
From what I have read, you want to be over 8% on the Omega-3 index and below 2.0 on the TG/HDL-C ratio.
Some articles:
Blood levels of long-chain n-3 fatty acids and the risk of sudden death (2002)
https://pubmed.ncbi.nlm.nih.gov/11948270/
Circulation: Fasting Triglycerides, High-Density Lipoprotein, and Risk of Myocardial Infarction
https://www.ahajournals.org/doi/full/10.1161/01.cir.96.8.2520?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
Higher blood omega-3s associated with lower risk of premature death among older adults
https://www.hsph.harvard.edu/news/press-releases/higher-blood-omega-3s-associated-with-lower-risk-of-dying-among-older-adults/
Hi Doc! Curious about what you think of an APO-B of 113, yet an Lp(a) of 9 ? That seems to be contradictory.
I recently had an NMR which showed LDL-P of 1527 (a year earlier it had been 1100). Also small LDL-P of 605 , when it had been 226 a year earlier. The APO-B number was done for the first time only a few days ago. I’m 72, Type 1.5 diabetic (hba1c of 6.0 on metformin 500mg ER, bid), rheumatoid arthritis (although after 25 years, it suddenly seems to have disappeared). CAC score from 2 years ago of 420 (370 in LAD), 50 in another artery, and 0 in the other two). HDL – 53, LDL-C 109, Triglycerides 95 (were 66 a year earlier), Total Chol 179.
I eat a fairly low carb, high fat diet (20% protein, 20% carb s, 60% fat). Mostly healthy fats (sardines, various nuts, salmon, 90% dark chocolate) Some red meat, but not much. Some chicken). Walk 4+ miles a day at 3.5-4mph pace. Take Coq10,fish oil (1200epa,650dha),l-carnitine,Aged Garlic Extract, K2 (large amounts), Magnesium glycinate/lysinate chelate, Quercetin,Curcumin.
Curious why those numbers would have jumped in 1 year? The only other thing I can think of is that I discontinued my biological drug (Enbrel) about 4 months ago due to some issues with nerve/muscle twitching in my legs. Not sure if that was causing it, but RA doesn’t seem to be returning despite being off the drug. However, I’m pondering if it could have been reducing inflammation and thus keeping small dense particles at bay? Is that possible? Since I was non-fasting at the time of the NMR (which was a mistake, I believe), I’m going to consider redoing the NMR to see what the numbers would be. Since I haven’t changed my diet, the discontinuation of Enbrel seems to be the only other factor I can think of.
Have had no heart issues as of yet. Echocardiogram 2 years ok was ok. Ultrasound of carotid arteries was clear, Ultrasound of leg arteries (for nerve/muscle twitching) was clear. hs-CRP – .76
I’m 5’9″, 148lbs. Slender frame. Not on statins due to NNT and NNH not sounding very beneficial and being concerned of worsening diabetes from them and possible muscle issues that could halt my walking (which I find imperative to controlling my diabetes)
Thanks for any input you might have the time to share. Appreciate you and the efforts you make to educate all of us.
Mark