Time makes us fat. It’s not a myth, it’s a biologic fact. When we get old we get fat. In December 1863, William Banting, an English undertaker who went to great lengths to treat his own obesity, wrote in his now famous Letter on Corpulence: … For I have been generally informed that corpulence is one of the natural results of increasing years...”
Of course getting fat wouldn’t be an issue if it didn’t affect our quality of life and our risk of disease. Banting also wrote: … “Yet the evil still increased, and, like the parasite of barnacles on a ship, if it did not destroy the structure, it obstructed its fair, comfortable progress in the path of life”.
However, obesity’s association with aging does not mean that getting fat with all its dire consequences is inevitable. In fact we know that some people never get fat, and some people get fatter than others. Nonetheless, although there are genetic influences and other factors we can’t control, we have to understand that to a great extent it’s about how we live our lives.
It’s well documented that obesity is associated with increased risk of high blood pressure, lipid disorders and type 2 diabetes, the three hallmarks of metabolic syndrome. However, keep in mind that although obesity travels with these conditions, it’s not necessarily their underlying cause.
Sometimes we tend to focus too much on obesity as a problem by itself. If we look at it a bit differently, it appears that some aspects of modern lifestyle, together with a number of known and unknown environmental and genetic factors, have created a metabolic disorder with multiple consequences, one of which is obesity. Other consequences of this disorder, apart from the hallmarks of metabolic syndrome, are cardiovascular disease, non-alcoholic fatty liver disease, polycystic ovary syndrome, cancer and dementia.
Metabolic Syndrome and Insulin Resistance
If William Banting was alive today we would probably have diagnosed him with metabolic syndrome. He had no family history of obesity and did not consider himself lazy or inactive, and yet obesity crept upon him in his thirties.
The first description of metabolic syndrome can be traced back to Eskil Kylin (1889-1975), a Swedish physician and scientist who described a cluster of conditions, including high blood pressure, high blood sugar, obesity, and high levels of uric acid which can lead to gout. This was later to be named syndrome X or more commonly the metabolic syndrome.
The five conditions described below are used to define the metabolic syndrome. Three of these must be present in order to be diagnosed with the condition.
- A large waistline.
- A high triglyceride level in the blood.
- A low HDL cholesterol level in the blood.
- High blood pressure
- Elevated blood sugar
Metabolic syndrome is not a rare disorder and its prevalence has been growing fast. It is believed that 70 million Americans suffer from this disorder.
In his Banting lecture, at the American Diabetic Association’s annual meeting in 1988, Gerald M. Reaven proposed insulin resistance as the underlying factor in metabolic syndrome. Since then it has been acknowledged that insulin resistance plays a key role and the term “insulin resistance syndrome” has been used by some specialists.
Insulin is a hormone secreted by the pancreas. It plays an important role for the metabolism of dietary carbohydrates. Insulin resistance is defined as a diminished response to a given concentration of insulin. Most people with insulin resistance have elevated levels of insulin in their blood.
When the actions of insulin are impaired, carbohydrate metabolism becomes abnormal. This condition has been termed carbohydrate intolerance. It reflects the impaired ability of the body to metabolize carbohydrates when insulin resistance is present.
In his book, Why We Get Fat: And What to Do About It, Gary Taubes arguments that insulin plays a key role for the accumulation of fat in the body; … “First, when insulin levels are elevated, we accumulate fat in our fat tissue; when these levels fall, we liberate fat from the fat tissue and burn it for fuel”, … “Second, our insulin levels are effectively determined by the carbohydrates we eat”..
The Role of Carbs
The figure below is from a recently published paper by Richard D. Feinman and coworkers showing data from NHANES (National Health and Nutrition Examination Survey) indicating a large increase in carbohydrate as the major contributor to calorie excess in the United states from 1974-2000. The absolute amount of fat decreased for men during this period and showed only a slight increase for women.
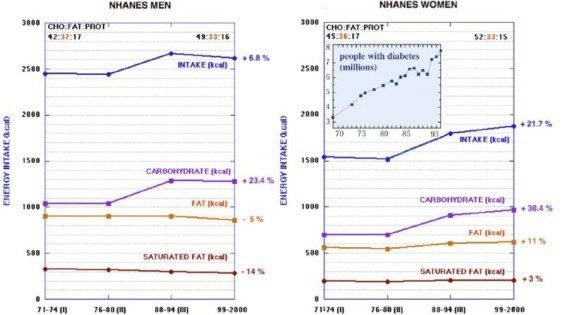
During the same time period, obesity increased dramatically and so did the prevalence of diabetes.
Today, 70% of adults in the US are classified as overweight or obese, as compared with 40% just 40 years ago. Whether the relationship between increased consumption of carbohydrates, and increased obesity and diabetes is causal or not is still a matter of debate. However the lack of any relationship between total and saturated fat consumption and the prevalence of obesity and diabetes is stunning.
However, to be fair, it must be emphasized that mortality due to coronary heart disease has dropped significantly in most countries during the last 40 years. Data on incidence are harder to find, particularly in the US, but evidence from many European countries suggests that incidence has fallen as well. So, fewer people are diagnosed with coronary heart disease and fewer people are dying from it. Nonetheless, the prevalence of heart disease is still very high. The population is aging and people often live with existing heart disease for decades.
Of course the dramatic fall in mortality due to coronary heart disease is due to multiple factors. Medical and surgical therapy has improved. Studies have also shown that less smoking, lower blood cholesterol and better control of blood pressure have all contributed markedly to lower mortality. Meanwhile however, increased prevalence of obesity and diabetes are working in the opposite direction.
What Do We Do About It?
The most effective way to solve a problem is to go for its roots. However, when it comes to the obesity epidemic and metabolic syndrome it gets complicated because we still don’t know, or at least we don’t agree, on the underlying causes. There are several potential contributors, among them are increased calorie intake, changes in the composition of our diets, less physical activity and changes in gut microbiome (the bacterial flora in our gut).
In a recent overview in The Journal of the American College of Cardiology, Carl J. Lavie MD and coworkers argue that progressive declines in physical activity over five decades have primarily caused the obesity epidemic. Their research has demonstrated very marked declines in occupation related physical activity and household management energy expenditure during the last fifty years.
Following the publication of Lavie’s paper, Larry Husten wrote an article on Forbes suggesting a possible conflict of interest. Husten writes: …”The article downplays the role of calories and diet and does not include the words “sugar”, “soda”, or “beverage”. Three of the five authors of the paper report financial relationship with Coca Cola.” …
Gary Taubes argues that we don’t get fat because we overeat. He believes it comes down to hormonal imbalance; … “the stimulation of insulin secretion caused by eating easily digestible carbohydrate-rich foods: refined carbohydrates, including flour and cereal grains, starchy vegetables such as potatoes, and sugars, like sucrose (table sugar) and high fructose corn syrup. These carbohydrates literally make us fat, and by driving us to accumulate fat, they make us hungrier and they make us sedentary”.
Public health organizations and medical societies usually advocate a low-fat, high carbohydrate, energy deficient diet to manage weight.
The American Heart Association believes we should approach metabolic syndrome by reducing our weight; increasing our physical activity; eat a heart-healthy diet that’s rich in whole grains, fruits, vegetables, lean meats and fish, and low-fat or fat-free dairy products and avoid processed food, which often contains partially hydrogenated vegetable oils, and is high in salt and added sugar.

In her recently published book, The Big Fat Surprise, Nina Teicholz writes about the changes in the American diet since the first dietary guidelines were published in the 1970s: … “Since the 1970s, we have successfully increased our fruits and vegetables by 17 percent, our grains by 29 percent, and reduced the amount of fat we eat from 43 percent to 33 percent of calories“…
Teicholz then reflects on the striking increase in obesity and diabetes in the US: … “In all it’s a tragic picture for a nation that has according to the government, faithfully been following all the official dietary guidelines for so many years. If we’ve been so good, we might fairly ask, why is our health report card so bad“…
Existing evidence indicates that carbohydrate restriction positively affects most of the essential features of metabolic syndrome. Weight loss is usually achieved, waistline is reduced, blood pressure is improved, triglycerides and HDL-cholesterol improve, there will be less insulin resistance, and glucose metabolism improves.
Despite the obesity epidemic occurring right in front of our noses, there is still disagreement on its fundamental underlying causes. Consequently, experts disagree on how to deal with it. Unfortunately, public health authorities have not been able to offer much guidance. Nonetheless, looking at all the available evidence, carbohydrate restriction appears to be an effective method to deal with lifestyle induced metabolic disease, and its consequences. However, unless medical professionals and health authorities acknowledge the potential of this approach, we can’t expect much success.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.


Excellent article!
“Existing evidence indicates that carbohydrate restriction positively affects most of the essential features of metabolic syndrome. …”
Compared to what? Compared to the typical, Western diet, no doubt. But a recent meta-analysis found “little or no difference in weight loss and changes in cardiovascular risk factors up to two years of follow-up when overweight and obese adults, with or without type 2 diabetes, are randomised to low CHO diets and isoenergetic balanced weight loss diets.” (https://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0100652#abstract0) I think the real key is adherence and the overall quality of the diet, not the macronutrient composition per se.
I would hesitate to take the NHANES data you refer to at face value. USDA data shows that added sugars accounted for 8 percent of the increase in available calories (loss-adjusted) for the last 40 years, while grains and added fats accounted for 40 and 50 percent of the increase, respectively. Calorie from fat increased with about 25 % from 1970-2009 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3849418/), and as Stephan Guyenet has shown on his blog, there is a strong correlation between the increase in fat intake and obesity prevalence (https://wholehealthsource.blogspot.no/2014/04/calorie-intake-and-us-obesity-epidemic.html).
By the way, longitudinal studies have found correlations between saturated fatty acids in plasma and tissue and type 2-diabetes risk, but this is hard to interpret (it may not reflect dietary intake of saturated fats).
Thanks for the comment Erik. I appreciate your input.
You‘re right, I wasn’t comparing carbohydrate restriction to other methods. That wasn’t really my purpose here. However, studies have shown some metabolic advantages of this approach, even when compared to low fat diets.
I suppose we all agree that weight loss is important for most people with metabolic syndrome. But,there are many ways to lose weight (we know most of them don‘t work by the way), carbohydrate restriction is just one of them. However, central obesity may be more important than BMI. I don‘t know whether you recall a Swedish paper showing that high intake of dairy fat was associated with a lower risk of central obesity and a low dairy fat intake was associated with a higher risk of central obesity.
You may also remember a systematic analysis from Sweden presented last year showing that low carb diets gave the best results short term in terms of weight loss. No adverse effects of carbohydrate restriction were found.
Interestingly the meta-analysis you cited, recently published in PlosOne defined “low carbohydrate” as less than 45% of energy consumption. Of course this cut-off is debatable. Many would not consider 40% percent carbs to be carbohydrate restriction.
Although we can‘t blindly rely on NHANES data, we can‘t ignore them either. In fact, fat consumption decreased in many European countries in the time period 1980-2000. At the same time the prevalence of obesity rose markedly.
Regarding Stephan Guyenet‘s article you cited, I think he was arguing that we‘re eating more of everything than we did 50 years ago, suggesting that it‘s mainly about calories.
As usual, I have to bring omega-6 into the picture. The switch from traditional (animal) fats to seed oils rich in linoleic acid is really the only alteration in the food supply that corresponds with the tremendous increase in heart disease, cancers, and other noncommunicable diseases. Yet, there’s almost no awareness or concern. Bill Lands, Joseph Hibbeln, and Fred Kummerow are among the few who get the connection. Excerpt from a Joseph Hibbeln Interview:
“Just as all polyunsaturates are not created equal, all high fat diets are not created equal. A good example of this is an animal study we did where we compared three high fat diets. All with 60% of calories from fat, in mice. We compared high fat diets that resembled the linoleic acid, Omega 6 intakes, comparable to the levels at the beginning of the century, which was about 1 percent of calories, and those high fat diets with 8 percent of calories, more similar to the amount of Omega 6 in the diet simply from soy oil in the U-S diet, today. Moving from 1% to 8% linoleic acid in the mouse diets, not only tripled the levels of arachidonic acids, but also tripled the levels of a critical derivative of arachidonic acids, which is an endogenous cannabinoid, which creates a similar affect to marijuana. So it’s the brains own marijuana like molecules, and we were able to triple the body’s marijuana like hormones, three times higher in the liver and about 20% higher in the brains just by altering the linoleic acid in those two high-fat diets. Normally those high fat diets used for mice in studies are composed of high linoleic acid, found in soybean oil. When we deleted that one single molecule, the Omega 6 fatty acid, we were able to obliterate the ability of a 60% high fat diet to induce obesity in the mice.” https://www.meandmydiabetes.com/2013/03/10/vegetable-oil-associated-with-more-heart-deaths-nih-scientist-joe-hibbeln/
Doc,
some of the best data sets showing staggering reductions in age-adjusted CHD mortality come from Finland, New Zealand, Sweden, Iceland, etc. In these countries the number 1 factor explaining plummeting heart disease rates have been changes in serum cholesterol which is again explained almost completely with the changes in the intake of saturated animal fats. In both New Zealand and Finland heart disease mortality rates (age-adjusted) fell around 80%.
In 1989 Epstein examined the changes in coronary heart disease mortality in 27 countries during the previous 10 to 25 years, noting that:
“In almost all of the countries with major falls or rises in CHD mortality, there are, respectively, corresponding decreases or increases in animal fat consumption…
Epstein also noted that during this period the prevalence of smoking among women remained largely unchanged or increased in most nations, and that therefore changes in smoking prevalence was unable to explain the large differences in the rate of decline between countries and sexes.
https://www.ncbi.nlm.nih.gov/pubmed/2681019/
Most diabetics and overweight people die in CHD related causes. I am not sure if LDL elevating low-carb diets make up a good solutions to tackle obesity rates. Amphetamine also result on weight loss and hence lower triglycerides (and boost HDL-C) without any adverse effect to number 1 causal factor for heart disease (LDL “bad” cholesterol, that is).
Low-fat, high-carb diet plus fish oil may improve overall insulin sensitivity and insulin sensitivity of fat tissue compared to low-carb diets. When Atkins money is absent the scholars do not need to construct “low-fat” straw men diets.
Effect of dietary fat modification on subcutaneous white adipose tissue insulin sensitivity in patients with metabolic syndrome.
https://www.ncbi.nlm.nih.gov/pubmed/25044988
My wife is 51 years old, a diabetic. She has the following lab numbers:
BP 110/70, Glucose 107, A1c 6.4, total cholesterol 180, Triglycerides 153, HDL 37, LDL 112. She is taking meds for diabetes and does mild exercise, no meds for cholesterol.
My question is what do you think about her lab results?
Thank you,
Miguel Jorge
Miguel. her cholesterol and LDL-C are quite ok. High TG/HDL-C ratio is often associated with insulin resistance which she obviously has (assuming she has type 2 diabetes). If she’s overweight or has abdominal/visceral obesity, losing weight is probably helpful. Regular exercise can improve HDL-C. Omega 3 can lower TG
Hi Miguel,
I like this video from Specialty Health. It’s a conversation of a case study of a Reno police officer between the head of Specialty Health, Dr. Thomas Dayspring and Gary Taubes. They talk about the risk factors the police officer exhibits and the treatment methods they undertook. I disagree about Dayspring’s insistence on the need for statins but I think it’s very informative on what risk markers have actual value and what treatment options are good to undertake.
https://www.youtube.com/watch?v=an6L9VY0v8A
So happy I found your blog. Seems I am guilty of this Metabolic syndrome..I am on three different BP meds, a statin and my doc says if I continue on the road I’m on I will be a full fledged diabetic in six months (glucose 115) no meds “yet”. I am also 75 lbs overweight. I am determined to get my life under control. I grew up addicted to sugar and although I do not eat much of sweets anymore I believe the damage has been done and I must stop the carbs.
On a side note..I am half Icelandic, US born and grew up on cream and jam filled Pönnukökur and my Grandmother made the best Kleinur bar none! I remember as a young child watching her drink her coffee, she would put a sugar cube between her teeth and sip the coffee through it! Again thanks for all the information you put out there.
Thanks for your comment Anna and for sharing your thoughts.
Pönnukökur and Kleinur are still popular here, of course their full of carbs. On the other hand we have to remember that the fact that carbohydrate restriction is helpful in metabolic syndrome does not necessarily imply that intake of carbs is the cause of this disorder.
Wish you all the best and hope your health will improve. I’m sure it will if you have a plan and are determined to stick with it.
Axel,
“Many would not consider 40% percent carbs to be carbohydrate restriction.”
Yet, this is what you get in the long-term dietary trials.
There’s a striking contrast between short-term low carb trials and long-term trials (e.g. Foster et al, Shai et al). Low carb is quite successful in the former – since the benefits come MAINLY from the weight loss which is bigger than in the control diets – whereas the differences become clinically negligible and/or statistically insignificant in the latter as the inevitable rebound takes place.
In other words, there’s no need for medical professionals to acknowledge anything else than the fact that low carb diets are one possible option. One size doesn’t fit all.
I absolutely agree Mie. Carbohydrate restriction should be acknowledged as one possible option. I hope I never implied anything else.
I have been on a high fat low carb diet for 6 years. After Hep C caused liver disease (fibroscan score of 11.8kpa – bridging fibrosis/cirrhosis) I was insulin resistant, napping 4 or 5 times a day and unable to get up the stairs without resting at the top. I was never really fat but my muscles had wasted and had been replaced by fat – my waist, hips and thighs were flabby. Within 6 months of going LCHF my LDL, HDL and Triglycerides were textbook – after a year my fibroscan score was 6.2kpa. Its now 5.8kpa. I swim 2 miles 3 times a week and participate in open water swim events. I work out with calisthenics and all fat has been replaced by muscle. I don’t nap any more – I don’t need to. I am 52, I have no idea what my weight is, I don’t need to know – I have a great figure. Getting fat is not a question of age, its a question of diet.