Estimated reading time: 7 minutes
The role of low-density lipoprotein cholesterol (LDL-C) in the evolution of heart disease is fairly well established. In addition, the benefits of pharmacological treatment with agents that lower LDL-C in high-risk patients are well documented.
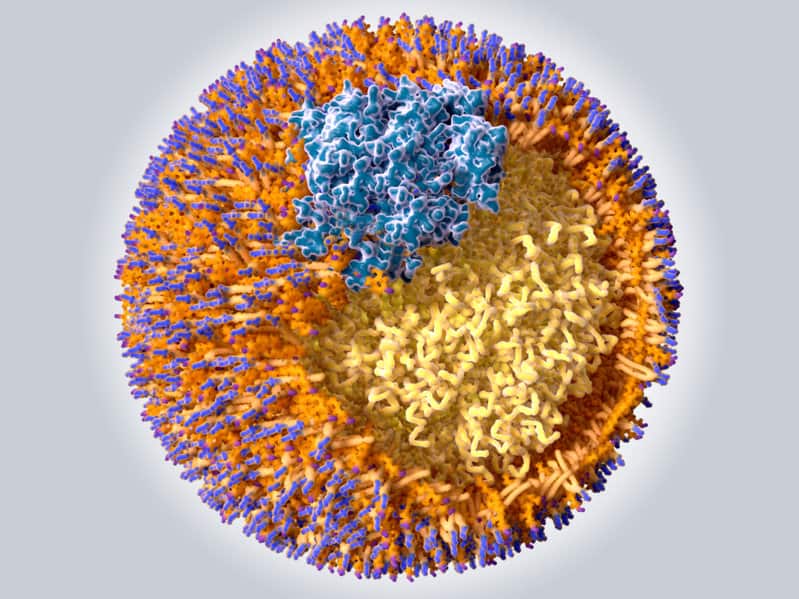
Lipoproteins are biochemical structures that enable the transport of lipids such as cholesterol in the circulation. LDL-C represents the amount or mass of cholesterol carried by low-density lipoprotein.
The interaction between circulating lipoproteins and the arterial wall is the first step in atherosclerosis and the development of heart disease. However, only some lipoproteins tend to interact with the arterial wall and trigger this bleak cascade of events (1). These lipoproteins are termed atherogenic. Low-density lipoprotein (LDL) is an atherogenic lipoprotein.
Today, there is ample evidence that the number of LDL particles (LDL-P) plays a much stronger role in the development of cardiovascular disease than the mass of cholesterol within these particles. This needs to be clarified because cholesterol mass does not always go hand in hand with the number of particles.
Furthermore, relying on LDL-C has several pitfalls (2). For example, LDL-C is a calculated variable that counts on measurements of total cholesterol, HDL-cholesterol, and triglycerides.
LDL-C does not accurately reflect the number of atherogenic LDL particles. This may explain why a large proportion of patients with cardiovascular disease do not have elevated levels of LDL-C.
Furthermore, clinical trials have shown that many patients who receive treatment with an LDL-C lowering drug and achieve a substantial reduction in LDL-C levels still develop clinical events (eg. heart attack or stroke)(3).
The LDL Particle
Lipoprotein particles are commonly classified according to their density, thus the terms high-density lipoprotein (HDL) and low-density lipoprotein (LDL).
There are six major types of lipoproteins; chylomicrons, very-low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and lipoprotein(a) (4,5,6,6).
LDL is called low-density lipoprotein because LDL particles tend to be less dense than other lipoprotein particles. Its main function is to deliver cholesterol to cells of the body.
Apolipoprotein B (apoB) is the primary lipoprotein in LDL (7). apoB-containing lipoproteins play a hugely important role in atherosclerosis and heart disease. All atherogenic lipoproteins contain one molecule of apoB.
A key step in the atherosclerotic process is the entrapment of apoB-containing lipoproteins within the arterial wall (8).
The Difference Between LDL-C and LDL-P
There is strong scientific evidence that LDL and other apoB-containing lipoproteins, including VLDL and their remnants, IDL, and LP(a), are directly implicated in the development of atherosclerotic cardiovascular disease (9).
Accordingly, a biochemical marker reflecting the amount of all these atherogenic lipoproteins would be of great clinical value when predicting the risk of heart disease.
However, despite its flaws, the assessment of the amount of cholesterol within LDL particles (LDL-C) is the most commonly used indicator of risk in the clinical world. Furthermore, LDL-C is also used to target therapy in primary as well as secondary prevention of cardiovascular disease.
Here, it is important to underline that LDL and LDL-C are not synonymous. In fact, the cholesterol content of LDL particles varies greatly. Hence, measurements of LDL particle number (LDL-P) maybe of importance (10).
Let’s take an example. Two patients with the same LDL-P may have very different LDL-C, depending on the amount of cholesterol within each LDL particle. However, their risk of developing heart disease may be similar.
Hence, LDL-C is a surrogate measure that only provides a very rough estimate of LDL particle concentration (LDL-P). Studies clearly indicate that the risk for atherosclerosis is more related to the number of LDL particles than the total amount of cholesterol within these particles (11).
It is also important to remember that LDL particles carry other lipid molecules than cholesterol. For example, triglycerides (TG) are also carried within LDL particles. Similar to total cholesterol and LDL-C, there is an association between serum TG and the risk of cardiovascular disease (12).
If the number of TG molecules in an LDL particle is high, there will be less space for cholesterol molecules. Therefore, if TGs are high, it may take many more LDL particles to carry a given amount of cholesterol. Therefore high LDL particle count may be associated with small, cholesterol-depleted, triglyceride-rich particles. Research has shown that high levels of triglycerides are associated with small LDL particle sizes (13).
So, what does all this mean? It means that one person (person A) may have large cholesterol rich LDL particles, while another (person B) may have smaller cholesterol-depleted particles. These two persons may have the same LDL-C concentration. However, person B will have a LDLP. Despite similar levels of LDL-C, person B is at higher risk four future cardiovascular events.
Many studies have suggested that the size of LDL particles may be of importance (14). People whose LDL particles are predominantly small and dense, have a threefold greater risk of coronary heart disease. Furthermore, the large and fluffy type of LDL may actually be protective.
However, keep in mind that the association between small LDL and heart disease reflects an increased number of LDL particles in patients with small LDL. Therefore, the LDL particle count could be more important in terms of risk than particle size in itself.
ApoB and LDL-P both reflect the number of atherogenic lipoprotein particles. However, measurements of ApoB will reflect the number of all atherogenic particles, whereas LDL-P only reflects the number of LDL particles.
Research shows that ApoB and LDL-P are better predictors of cardiovascular disease risk than LDL-C (15).
Discordance
Discordance is when there is a difference between LDL-C and LDL-P. If LDL-C is high and LDL-P is low, there is discordance. If LDL-C is low and LDL-P is high, there is discordance. If both are low or both high, there is no discordance.
Studies have indicated that if there is discordance between LDL-C and LDL-P, cardiovascular disease risk tracks more closely with LDL-P than LDL-C (15). Specifically, when a patient with low LDL-C has a level of LDL-P that is not equally low, there is a higher “residual” risk. This may help explain the high number of cardiovascular events that occur in patients with normal or low levels of LDL-C.
The “Get With the Guidelines” study published in 2009 reported lipid levels in almost 137 thousand patients with an acute coronary event (16). Almost half of those had admission LDL levels <100 mg/dL (2.6 mmol/L) which may be considered fairly low. Hence, LDL-C did not seem to predict risk in these patients. However, low HDL-C and elevated TG was common among these patients. Low HDL-C and high TG levels are generally associated with higher LDL-P (16).
Among discordant patients in the Framingham Offspring Study the group with the highest risk for future cardiovascular events had high LDL-P and low LDL-C, while the group with the lowest risk had low LDL-P but higher LDL-C (17).
Many patients with metabolic syndrome or type-2 diabetes have discordance where LDL-P is elevated but LDL-C may be close to normal. In these individuals, measurements of LDL-C may underestimate cardiovascular risk. Measurements of ApoB or LDL-P are much more likely to predict risk in these individuals.
Discordance may be an important clinical phenomenon. Sometimes the question of medical therapy in primary prevention arises when there is an intermediate risk, based on LDL-C. In these cases, a low LDL-P level might help to confirm that the risk is indeed low, which might justify avoiding statin therapy.
Statins tend to lower LDL-C more than LDL-P. Many individuals who reach the target for LDL-C with statins, may still have raised LDL-P. This may indicate a higher residual risk despite what is generally defined as adequate treatment.
The article was initially published in 2012
It was revised, updated and republished on August 24, 2022.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

Very nice post. Thanks clarifying this pretty complicated subject. How convincing is the evidence in your opinion that LDL-P should be the primary parameter to follow? Does it add anything on top of ApoB?
Thanks Reijo. The problem with the LDL-P measurements using NMR spectroscopy is that it is still rather expensive. It has been suggested that looking at non-HDL cholesterol (total cholesterol minus HDL cholesterol), HDL-C and triglycerides may be helpful when LDL-P and ApoB are not available. This could be important in patients with the metabolic syndrome, where LDL-C may underestimate risk. Non-HDL cholesterol reflects the cholesterol within all lipoprotein particles currently considered ateherogenic. Many studies have indicated that it is a better predictor of cardiovascular events than is LDL-C. However I still think LDL-P measurements may often give important additive information and I my guess is that it´s use will become more common in the near future. However, the clinical utility of these measurements is still limited because the technique is not widely available and it is relatively expensive.
In clinical terms, LDL-P does not add much to ApoB. LDL-P measures the number of LDL-particles while ApoB measures the number of all atherogenic particles (chylomicrons, VLDL,IDL,LDL and Lp(a)). Usually 85-90% of ApoB represent LDL-particles.Therefore, in most cases you don´t need ApoB if you have LDL-P available and vice versa.
I like your question Reijo. I hope we can get an answer. In my case I have discordance between APO-B and LDL-P. I’d sure like to know how that can happen. My APO-B is low-normal but LDL-P is “high risk” so nothing has been clarified for me as yet.
TRY THE BOSTON HEART TEST
I WAS ABLE TO GET A TEST FROM ONE OF THE “WALK IN” LABS WHERE YOU CAN ORDER YOUR OWN TEST. THIS TEST GAVE ME THE LDL-P ALONG WITH THE STANDARD LIPID RESULTS. THE PRICE WAS ONLY $58. LIPO SCIENCE IS PROVIDING ALL THE NMR RESULTS SO IT DOESN’T REALLY MATTER WHAT LAB DRAWS THE SAMPLE. THEY ARE ALL SENDING IT TO LIPO SCIENCE.
I DIDN’T GET ANOTHER APO-B FOR THIS PRICE HOWEVER.
“l…HD-CL and triglyserides …important in patients with the metabolic syndrome, where LDL-C may underestimate risk” Have you a solid reference to this statement? Would be very interesting as almost all the fuss is about LDL-C.
Reijo. Here is a study on the use of Non-HDL cholesterol to predict risk in patients with type-2 diabetes. It is a stronger predictor of risk than LDL-C. Another study arrived at the following conclusion: Non-HDL is a stronger predictor of CHD death among those with diabetes than LDL and should be given more consideration in the clinical approach to risk reduction among diabetic patients. Here is another study comparing ApoB and Non-CHDL cholesterol with LDL-C.
In this short video Dr. Richard F Wright explains discordance and the populations most likely to be at increased risk despite normal LDL-C. It turns out that that patients with diabetes often have high LDL-P despite normal LDL-C. Here Dr Thomas Dayspring explains why LDL-C is a much worse predictor of risk in insulin resistant patients than ApoB or LDL-P.
Excellent post. Here is another study: Cui Y, Blumenthal RS, Flaws JA et al.: Non-High-Density-Cholesterol Level as a Predictor of Cardiovascular Disease Mortality. Arch Intern Med. 161, 1413-1419 (2001).
Hi doc, any thoughts on the usefulness of TG/HDL ratios? I’ve heard that TG is a fairly accurate proxy for ApoB count. Plus TG numbers are easy to obtain. thx!
@ Richard. Evidence suggests that there is an association between TG/HDL-C ratio and cardiovascular risk. This ratio has also been shown to be associated with insulin resistance. Thus, the higher your TG and the lower your HDL-C, the greater degree of insulin resistance. Therefore it may be particularly helpful in individuals with the metabolic syndrome where the traditional LDL-C often underestimates risk.A TG/HDL-C ratio above 3.5 has often been used as cutoff for identifying insulin resistance. As you say, this ratio is easy to obtain, it is included in the traditional lipid panel, and therefore relatively cheap.
I get asked many times why the arterial wall gets damaged in the first place. I am also asked if this can be reversed – the implication being by non surgical/medicinal means.
I know smoking, insulin spikes etc. can lead to inflammation, but why does (rhetorical) the wall become weakened before this happens. Age? Yes possibly…… and yet I still seem to need to dig deeper, especially when arterial damage was detected in me at the age of 49 years – not particularly ancient!
Have you ever considered the Rath – Pauling theory? Explained here by Dr. Dach.
https://www.drdach.com/Heart_Disease.html
Curious and also wondering what your treatment regime would be for natural reversal of plaques?
Clare in Tasmania
As far as I know the only attempt to establish a logical hypothesis of atherosclerosis explaining at least a big chunk of observed data is the one by Drs. Ravnskov and McCully where damage is first inflicted in the vasa vasorum: see for example Infections May Be Causal in the Pathogenesis of Atherosclerosis (available at last International Health News issue). For me confusing correlation with causation (LDL-P hypothesis?) and ignoring how LDL particles jump through supposedly healthy tissue doesn’t cut it.
This being said I am all in for vitamin D, magnesium, vitamin C, vitamin K2, iodine etc.
This article was hugely helpful albeit upsetting for me. I am a very fit 38 y/o male; I bike race and have always enjoyed a high carbohydrate/low fat diet. After getting the VAP test, it turns out my LDL-P is 1733 nmol/L !! Total Chol is 202, LDL-C Direct = 127, HDL-C = 63, TG’s=104. My father has CAD. I took Lipitor for 40 days and developed severe, debilitating muscle pain in my wrists, forearms and biceps. After 2 weeks off it I can start to pick up my 6 mo. old son again. I’m terrified of the statin drugs but do I have no other choice? Should I restrict CHO’s? Should I get a more specific test like the NMR LipoProfile? Thank you for responding.
Lipitor 95% ineffective but it may lower your LDL-c.
Try a higher fat diet instead of high carb diet. The carbs may be causing inflamation. People are way too antifat. Just keep the calorie levels within needed limits. At least limit the carbs try around 100g a day and get therest from high protein medium fat diet. Get much of the carbs from fruits and veg as possible. Then test in 6 months. Fatty fish nuts etc but also meat fat i truly believe has benefit especially when eaten with veg and tje meat and nutrients it comes with.
Sometimes bro science works better than medical science. Because they are slow to adopt new natural treatments and focus on only what they can prove over time clinically.
Great article. Very helpful in understanding LDL-P. I have high LDL-C, LDL-P, and apoB. In addition, I was tested and told my LDL are the “large and fluffy” ones. Yet I still have damage. I have about 60% blockage in my carotid- so atherosclerosis is there despite my LDL size. I’m trying to understand the cardiac risk relationship of LDL-P and the size of the particles. I keep reading “large and fluffy” LDL is not suppose to be harmful (or as the link above says “relatively benign”). I don’t see how that is true- looking at my own labs. Can you shed some light on this or provide additional links that don’t just explain what size is but the thinking/facts/studies behind the larger size and lower risk factor? At some point does high LDL-P negate the size and size no long becomes protective or benign? Do we know those tipping point levels or have answers to these types of questions yet? Thanks so much!!
BTW I’m only 42 and been vegetarian most my life and am active. I’m getting genetic testing to confirm probable FH or FDB.
@ Dan – I can’t tolerate statins either and need more than lifestyle to lower my Total Cholesterol, LDL-C (my TG are normal). I’m in a clinical trial for a new drug that lowers LDL-C levels (I don’t know if it lowers LDL-P and/or apoB too). It doesn’t appear to have the muscle degrading problems that people experience on statins. It’s still in it’s trial stage but seems promising. You may want to look into it – it’s a PCSK9 inhibitor.
Try eating a different diet. Carbs are maybe the culprit elevating insulin levels and affecting hormones. I personally dont agree with the so called science behind vegitarian diets.
I mean your unhealthy so maybe try a new diet for 6 months. Low carb high protein relatively higher fat and variety of foods.
60 year old woman. Had the very expensive blood tests. The results of my tests are all over the place.
total cholesterol: 184 (optimal)
LDL-C: 116 (intermediate risk)
HDL-C: 56 (optimal)
Triglycerides: 82 (optimal) under 150 is optimal, so mine are great
Non-HDL_C: 128 (optimal)
sdLDL-C:20 (optimal)
All looks great. BUT …
ApoB: 94 (high risk)
LDL-P: 1596 (high risk)
Lp(a) Maa: 73 (high risk)
Lp(a)-P:268 (high risk)
From what I read, Lp(a) is genetic and nothing I can do about it.
From your article, looks like I have “discordance” and I’m not the typical patient. Triglycerides are opposite of ApoB and LDL-P.
sdLDL-C being 20 looks like I have few small, dense LDL particles. That is great. But LDL-P is 1596, which means I have LOTS of LDL particles, and that isn’t good. And APO-B is total of ALL atherogenic particles, and mine are very high.
Have not had any cardiac incidents and have no idea what my arteries look like.
What to do …. what to do ….
Enjoy your life. Stop stressing about it
Probably stress will cause more risk for heart disease than your numbers. It especially affects stress related hormones and that is bad.
i had a heart attack 6 years ago , i went through a bypass operation and had to change 4 arteries that were totally blocked .
My cholesterol levels were normal and my sugar level was good so i never knew the reason for what happened .
Last week ( six years later ) i made this test showing the LDL-P and was shocked to learn they are above 2000 despite normal LDL-C (91) normal triglycerides levels (116 ) & normal total cholesterol (158)
So i guess the LDL-P is the most important indicator to assess a risk factor , i am on Crestor 20 but it doesn’t seem to have any affect of it , My Dr has added Zetia 10mg and i will see its effect in my next blood test 3 months from now .
is this conversation still active in November 2014. If so I’d like to join
Eve.
Feel free to share your thoughts.
Peter Attia says apob is a good proxy for ldlp. What would be a good range for apob?
David
Regarding apoB:
Usually less than 100 mg/dL is considered desirable in low or intermediate risk individuals.
Less than 80 mg/dL is desirable in high risk individuals, such as those with cardiovascular disease or diabetes.
https://www.docsopinion.com/health-and-nutrition/lipids/apolipoprotein-b-apob/
I see in my practice all to common, people hold a false security. Their LDL-p still lives above 1500 and their CRP> 5 and their HbA1c > 6.
I belive it is like carmolizing an onion. The inflation is the heat, which causes the sugar to damge the endothelial tissue, which allows the LDL-P to infiltrate – thus causing plaque to accumulate.
Metabolic syndrome seems to be the perfect storm for CAD creation.
I have also witnessed the lowering of LDL-P by 50% in 4 weeks by eliminating homoginted fats from the diet and adding avicodo and almonds.
Overall I’m of the opinion that statins are over rated and encourage a false seance of security – the American Dream.
Dear Dr Sigurdsson,
I have had very discordant lipid profile tests over the past few years. I’m 35 yrs old Male with family h/o MI in my father @ 65 yrs of age (he had poorly treated high LDL-C and HT). My mother has typical metabolic syndrome.
I have Gilbert’s syndrome (supposedly associated with high HDL and low CAD).
~5 yrs ago, I had a HDL of 76 mg/dl, LDL of ~ 55 mg/dl and Total Cholesterol ~ 150 with low TG. I was exercising regularly and was quite fit (nowhere near a college athlete).
With the VAP test in Nov 2013, My profile was (non- fasting)
Total cho: 194, LDL-P 2181 !!! TG- 249 HDL only 60!, LDL total- 106, Apo B 95, Apo A1 167,
IDL- 9, Total VLDL- 27, VLDL3- 12. LDL density pattern buoyant.
I wasn’t as fit but by no means overweight,etc with good diet. I couldn’t believe and I rechecked with my family doc, who could only do a routine profile and now the values for HDL are off again.. HDL ~ 55 or something.
I have 3 questions:
1) HDL usually remains constant and is genetic (as far I know) + Gilbert’s have high HDL. So why my HDL is fluctuating to this extent.
2) How can the LDL particle count be so high although the TG aren’t that high.
3) Is a low density LDL (buoyant) associated with a lower or a higher risk for CAD?
I apologize for a long post but could’nt make it shorter. Thank you very much.
So right and well described. I was trying to explain this to my Japanese doctor but unfortunately hes too old and my Japanese is not good enough. Medical practice is behind clinical research. He saw elevated LDL-C and was wondering why i wouldnt want to take statins. No further testing or diet was suggested. I am also a eeightlifter with 13% body fat and 44years old. Tg and HDL were normal. But of course my BMI says im obese because i have muscle mass- 74kg and 5foot7.
“Medical practice is behind clinical research” Wow. What an understatement. Thats the whole reason for this thread.
Very nice description!
could be more concise at the outset, just defining each one in first paragraph so we don’t need to wade through it to extract the information.
If both are low or both high, there is no discordance.So does this mean I can use ldl-c as my marker??And if not why?Thanks Doc
Exactly Vince. If there is no discordance, LDL-C will tell you what you need to know.
Thanks Doc…I have been getting the NMR for 3 years now and every time my ldl-c went up or down my ldl-p followed…latest ldl-c was 73 ldl-p is 722.
Nice post. Any thoughts on trig/ HDL as an indirect indicator for LDL-C/P? thx. Nick
Thanks.
Here’s a post I wrote on the issue of TG/HDL-C ratio as a marker of LDL particle number and size https://www.docsopinion.com/2014/07/17/triglyceride-hdl-ratio/
Nicely written article – thank you!
My Question is when there is a discordance between LDL P and ApoB? Would you try therapies to address LDL P?
Total Cholesterol 172
Trigs 31,
LDL C (NMR measured) 97,
HDL 78
Non HDL Cholesterol 94
ApoB 80 and LDL P 1300
This is lean male, 40s, exercises and on low carb diet, either in ketosis or flirting with it at all times. And is not main lining saturated fat…although it is present in diet
Thanks again!
is that chat still active?
Sure it’s still active.
i did a lot research in the field
What is the VAP test? I do keto – healthy fats only, very low carbs. My A1C is well within normal levels, where it was high before I started keto. Of course my doctor want to put me on statins. I’m not at all convinced that I need them and would like to learn more about what my numbers actually mean.
My fasting results are:
Component Your value Standard range
Cholesterol 292 mg/dL 0 – 199 mg/dL
Triglyceride 105 mg/dL =40 mg/dL
LDL, Calculated 212 mg/dL <130 mg/dL
Non HDL Chol, Calculated 233 mg/dL <=159 mg/dL
Cholesterol/HDL Ratio 4.9
Hi! I’m a 51 year old female. 5’6″ 132lbs. Fit and exercise. My Dad, an ER physician with about the same build, died at 51 after a jog, was on statins with cholesterol about 210 and the autopsy showed 98% blockage (occlusion?) and possible prior heart attacks he didn’t know about. Mother just had a triple bypass at 70. Bad family history. My Dad and I have been watching my cholesterol since I was 16 yrs old. Generally heart healthy diet..rarely have cheese or creams, never vegetable oil….only olive oil…. No clue what has caused this recent spike except I have been cutting back on red meat eating turkey and chicken. I have not gone through menopause yet. Any ideas? Oh, my calcium score on the X-ray was 0. I’m pretty scared about these latest numbers.
I just had the following results from NMR lips Profile
LDL-P: 1695 (in 2018 was 1258)
LDL-C: 134 (in 2018 was 109)
HDL-C: 91 ( in 2018 was 77)
Trig: 119 (in 2018 88)
Total Cholesterol: 245 (was 204 in 2018
Small LDL-P <90 (same in 2018)
HDL-P 38.5 (in 2018 was 35.3)
LDL size 22.1 ( in 2018 was 22.3)
I am insulin resistant and am on a low carb, higher fat, moderate protein diet and have been most of the past 4 years. Before I was put on statins, I was keto for 9 months, and my TG were down to 70, I still got LDL-p of 3000 and ApoB of 183 and ApoA of 168. LDL was 254. Then I got put on lower dose of crestor. It brought everything down, but still discordant. LDL of 99, LDL-p of 1600 and ApoB of 115. Will things possibly work themselves out if I lose the remaining 30 lbs I need to lose? I am down 20. Or do I need to cut the saturated fat down and add more other types of fat instead? It’s a mystery.
LDL Vs. TG/HDL
Two Case Histories
Lipid Panel 63 Year-old Woman (1) Tim Russert (2)
TC 311 159
LDL 215 67
HDL 73 32
TG 114 300
TG/HDL 1.6 9.4
TC/HDL 4.3 5.0
Notes:
(1) Given her high LDL’s, an artery scan was performed, which showed totally clear arteries—presumably because of the low TG/HDL Ratio, indicating that the LDL particles were the large, Type “A,” non-damaging type.
(2) Formerly with NBC News, died in 2008, from a massive heart attack, with a corrected cholesterol level, taking statins (see comment below). His sky-high TG/HDL Ratio indicated an immediate risk of a heart attack, because his LDL particles were predominately the small, Type “B,” damaging type, based on his TG/HDL Ratio.
A quote by Professor Abramson, a Harvard Medical School professor and physician:
“You can lower cholesterol levels with a drug, yet provide no health benefits whatsoever,” Abramson says. “And dying with a corrected cholesterol level is not a successful outcome in my book.”
Thanks Jeffrey.
I think you are underlining tow important points here.
Many post-menopausal women have high LDL-cholesterol but no arterial disease.
The second case reflects very well what is traditionally called residual risk. The high TG’s and low HDL-C may indicate small LDL-particles. Furthermore, triglyceride rich lipoproteins and remnant cholesterol may have played a role as well.
https://www.docsopinion.com/vldl-triglyceride-remnant-cholesterol/
Re: <<The “Get With the Guidelines” study published in 2009 reported lipid levels in almost 137 thousand patients with an acute coronary event (16). Almost half of those had admission LDL levels >
Do you have access to the TG/HDL data and if so, can you post the data?
Hi Jeffrey
Sorry, I don’t have access to these.
Axel
Here’s a link to the “Get With the Guidelines” study:
https://c065cd76-ef13-4ded-b3be-f2c0bc30d71e.filesusr.com/ugd/dfd979_6b7c74b5723e4f8a8fe1ec0a37d7966b.pdf
Doc, I wonder if you could contact the authors of the study and ask them to provide a table showing the TG/HDL Ratios? They obviously have the TG and HDL data, but they are shown in different charts. If I’m interpreting Table One correctly, it looks like the average TG/HDL Ratio was about 4.0.
Hello Dr. Sigurdsson;
I always enjoy your articles. I have a couple of questions for you:
1) Why are statins always recommended if you have high LdL-C but also a high number of Ldl particles? My understanding is that statins can reduce the amount of cholesterol produced but does it reduce the number of lipoproteins?
2) Would you know of any studies that confirm people with high Ldl-C, but low Triglycerides and high Hdl having heart disease?
Hi Brenda.
Thank you for the comment and for reading my articles.
1) Statins lower both LDL-C and the number of LDL-particles. However, there is evidence that in patients with metabolic syndrome, the magnitude of
LDL particle concentration reduction with statins is smaller than that of LDL
cholesterol reduction, suggesting that LDL cholesterol may underestimate residual risk in these patients. Hence, residual risk remains high despite statins.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2681027/
2) I don’t know if this question has been addressed specifically in any study. However, although the role of HDL-C has not been completely clarified, many clinical guidelines now recommend using non-HDL cholesterol instead of LDL-cholesterol when assessing risk. Non-HDL-C will reflect the amount of cholesterol carried by all apoB-containing particles. Of course it still only tells you about the mass of cholesterol and not the number of particles. https://www.docsopinion.com/non-hdl-cholesterol-non-hdl-c/
Hello Doctor,
I had some bloodwork done with a holistic doctor back in October last year – I don’t want to take statin. However, some of the results look a little scary: LDP-P: 2247 / LDL-C: 220 / Triglycerides: 83 / Total cholesterol: 300. Also, LDL size: 22.3. In your opinion, am I playing Russian Roulette with my life? I am 53 years old female and overweight (184lbs). Never smoked and I never drink. Never followed any specific diets but I do try to eat healthy most of the time – unfortunately, I do have a Sweet Tooth. I seldom exercise. Have an 8 to 5 office job. Went from 145lbs in my mid-forties to 184lbs now. What would you recommend? Thank you for any guidance.
Hello Elizabeth
I’m sorry for not being able to give you any personal advice.
This blog is for general informational purposes only and does not constitute the practice of medicine, nursing or other professional health care services, including the giving of medical advice, and no doctor/patient relationship is formed.
Elizabeth, i am not a doctor but i fee your pain. First, educate yourself as much as possible. We have the vast knowledge of the world at our fingertips but we all stare at memes all day. lol. What most people consider a healthy diet is what is killing them. Throw out that outdated and disproven food guide pyramid. All that has done since it’s inception is send hundreds of millions of people to their graves. You absolutely must ditch all processed foods and sugars from your diet. It isn’t a sweet tooth. Don’t sugar-coat it. 🙂 It’s an addiction. Plain and simple.
I suggest starting with Dr Jason Fung and Dr Sten Eckberg to learn what insulin resistance is… Fasting or not, they are very accessible and very informative. Read or watch youtube lectures from Dr Gary Taubes, Low Carb Down Under, Dr Fung, Dr Chaffee, Metabolic Mike (High intensity Health)… way too many to mention.
Most of all don’t believe anything someone can’t backup with a reference to a Published, Clinical trial that has been peer reviewed. Never take health advice from politicians or any company that profits from you being fat or chronically ill. Best of luck! -CL
Hello Dr. Sigurdsson!
How do you think – what is the right tactic: a lot of women have high Cholesterol and LDL at the age 43-55 and absolutely clean brachiocephalic arteries + САС = 0.
At the same time, cholesterol/LDL value often ~ 300/>200 mg/dl resp. For example, I now have several such patients now. Additional data does not provide clarity: CRP in the range 0-1,5; HbA1C – normal, they does nor smoke and TG 200 I must prescribe statins… But the question – for what – to adjust the ciphers?..
What should you do in this case, I really appreciate your opinion.