Estimated reading time: 12 minutes
Understanding Heart Palpitations: A Cardiologist’s Perspective
It often begins in the quiet.
You’re lying in bed, winding down from the day. Maybe you’re reading, perhaps just drifting off.
And then, your heart leaps.
A flutter.
A jolt.
A sudden thump that wasn’t there a moment ago.
Your mind scrambles: Was that a skipped beat? Is something wrong with my heart?
You’re not alone.
As a cardiologist, I’ve spoken to countless patients who’ve asked the same questions, often with anxiety in their eyes and a hand pressed to their chest. The sensation is real. And for many, it’s deeply unsettling.
But here’s what I always tell them:
Palpitations are common. Most are harmless. But a few deserve a closer look.
This article will guide you through the causes of palpitations, when to be concerned, and how we evaluate them in the clinic, drawing on a combination of medical science, practical insight, and lessons from real-life cases.
So, let’s begin with the basics.
What Are Heart Palpitations Exactly?
Palpitations are an awareness of your heartbeat, often described as something abnormal, intrusive, or unsettling. And while textbooks list the usual culprits—pounding, racing, skipping—it’s the way people describe them that truly brings the experience to life.
One man told me it felt like “a bird trapped in my chest.” A woman in her thirties said, “It’s like my heart tries to leap ahead of me and stumbles.” A teenager once said it felt like “a drumbeat echoing in my ears.” Others speak of a hiccup, a lurch, a pause that pulls their attention inward, followed by a heavy, compensatory thud.
These sensations can be brief—gone in a blink—or linger for minutes. They might strike during a quiet moment, or just as easily in the middle of a run or a heated conversation. Some patients feel them like clockwork at bedtime, while others say they arrive uninvited, like a wave washing over the chest and neck.
What’s remarkable is how personal it is. Some patients feel every tiny fluctuation in rhythm, while others can have irregular heart rhythm for days without noticing a thing.
Palpitations are a symptom, not a diagnosis. They can arise from the heart itself, but stress, hormones, posture, or perception can also shape them. That’s why no two stories are the same. And why the first step in evaluating them is always to listen—closely—not just to the heart, but to the narrative around it..
What Causes Palpitations?
When people feel an unexpected jolt or flutter in their chest, the instinct is to suspect a heart problem. And while the heart can certainly be involved, many palpitations have nothing to do with structural heart disease or dangerous rhythms.
In fact, some of the most common causes are non-cardiac. Over the years, I’ve seen countless patients who trace their palpitations to daily stressors, lifestyle choices, or metabolic shifts.
For example, someone struggling with panic attacks may experience a pounding heart even when their rhythm is perfectly normal. Another patient, worn down by poor sleep and too many cups of coffee, may feel flutters at night after finally lying still.
Here are some of the usual suspects:
- Anxiety and panic disorders: A racing heart is often the body’s natural response to fear, even when there’s no external danger.
- Caffeine, nicotine, alcohol: Stimulants can heighten heart sensitivity, especially in those already prone to palpitations.
- Sleep deprivation or emotional stress: Chronic fatigue and mental strain disrupt autonomic balance, causing the heart to beat faster or irregularly.
- Thyroid dysfunction (especially overactive thyroid): Excess thyroid hormone speeds up metabolism and heart rate.
- Anemia (low blood count): The heart may beat harder or faster to compensate for reduced oxygen delivery.
- Fever, dehydration, or low blood sugar: Each of these stresses the body’s homeostasis and can provoke a reactive change in rhythm.
- Certain medications or stimulants, such as decongestants, asthma inhalers, and some supplements, may trigger sensations of palpitations.
- Recreational drugs like cocaine or amphetamines: These can directly affect the heart’s electrical system, sometimes dangerously.
Of course, the heart itself can also be the culprit.
Some palpitations do stem from underlying cardiac conditions:
- Arrhythmias (irregular rhythms): Including atrial fibrillation, supraventricular tachycardia (SVT), and ventricular tachycardia.
- Valvular heart disease: Leaky or stiff valves can increase strain on the heart.
- Cardiomyopathy: When the heart muscle is weakened or thickened, it becomes more prone to irregular rhythms.
- Coronary artery disease: Reduced blood flow to the heart can occasionally trigger rhythm disturbances.
Here’s the twist: many people with significant arrhythmias feel absolutely nothing. Many people with strong, distressing palpitations are found to have normal ECGs and healthy hearts.
That’s why clinical context is everything. We must listen to what the heart says—but also how the patient tells the story.
An arrhythmia simply means your heart isn’t keeping a steady rhythm. It might beat too fast, too slow, or with unexpected skips and stutters. Some arrhythmias are harmless and come and go. Others may signal something more serious. Part of the challenge—and the art—is figuring out which is which.
The Heart’s Electrical Highway
To understand palpitations, it is essential to comprehend how the heart regulates its rhythm.
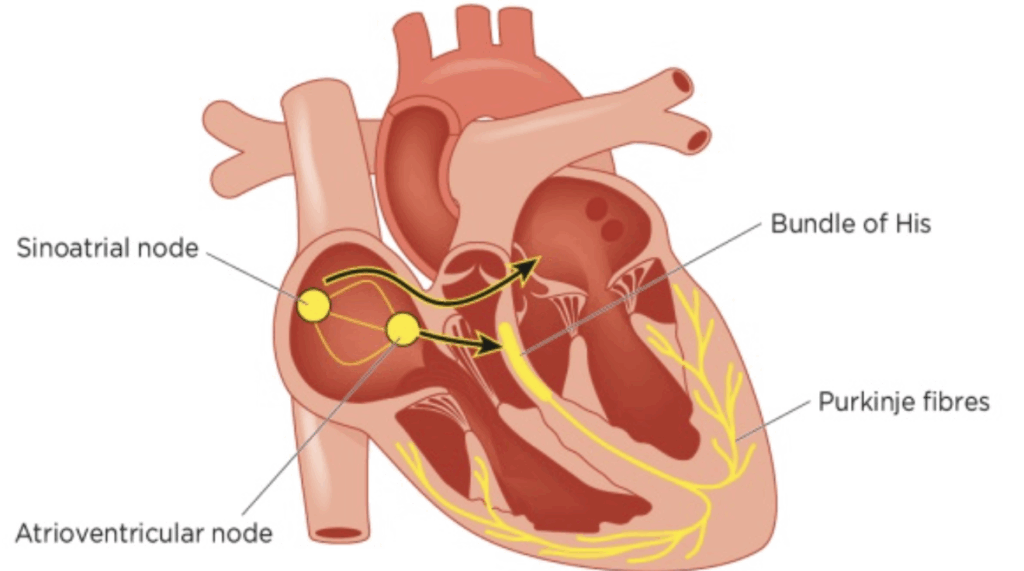
The heart has its built-in pacemaker, the sinus node (SA node), located in the upper right atrium. Like a conductor setting tempo, it sends out electrical signals—more than 2.5 billion over a lifetime—guiding the synchronized contraction of the atria and ventricles.
Normal heart rhythm originating from the sinus node is termed sinus rhythm.
Next, the signals travel to the area that connects the atria with the lower chambers of the heart (the ventricles), the atrioventricular node (AV node), and from there through an area called the AV bundle or the bundle of His.
The bundle of His splits into thinner branches (right and left bundle branches) that extend to the right and left ventricles. Finally, the signals reach the muscle cells of the ventricles, causing them to contract.
A normal resting pulse usually varies between 40 and 100 beats per minute. The sinus node, influenced by signals from the nervous system and endocrine organs, constantly adjusts the heart rate to meet demands, such as during physical exercise.
It’s a beautiful sequence—until something interrupts it.
Disruptions can cause the heart to beat too early (a premature beat), too fast (tachycardia), too slow (bradycardia), or erratically (fibrillation). Any of these can lead to palpitations.
When Rhythm Breaks the Rules: Ectopic Beats and Arrhythmias
Sometimes, the heart throws in a beat that feels out of place. These are called ectopic beats, and they’re incredibly common. Most of us experience them at some point, often without even knowing it.
Ectopic beats are classified based on where in the heart the extra electrical signal originates. They fall into two broad categories:
Ectopic beats fall into two broad categories:
- Premature atrial (supraventricular) contractions (PACs)
- Premature ventricular contractions (PVCs)
They’re extra beats that occur before the next normal beat is due. Many patients describe them as a “pause,” followed by a stronger beat, because the heart fills more before the next contraction.
The good news? They are typically benign, particularly in people with healthy hearts. Most patients with these forms of ectopy have an excellent long-term outlook and require little more than understanding and reassurance.
That said, when these ectopic beats occur frequently or in runs, they may form more sustained arrhythmias:
- Supraventricular tachycardia (SVT) — A fast rhythm from the upper chambers, often starting and stopping abruptly
- Ventricular tachycardia (VT) — A rapid rhythm from the ventricles; concerning if sustained or linked to heart disease
- Atrial fibrillation (AFib) — An irregular, often rapid rhythm that increases stroke risk
Supraventricular tachycardia is relatively common. Although the prognosis is usually good, this arrhythmia commonly causes palpitations, and specific treatment may be needed to relieve symptoms.
Ventricular tachycardia may cause dizziness and fainting. The prognosis is usually good if it lasts less than 30 seconds (non-sustained) and is not associated with underlying heart disease.
However, ventricular tachycardia may sometimes be associated with an adverse prognosis and risk of sudden death.
Atrial fibrillation is a common underlying cause of palpitations. It is characterized by chaotic electrical activity of the atria, leading to a rapid and irregular heart rhythm. Atrial fibrillation is sometimes associated with an increased risk of stroke.
But how do we distinguish between the harmless and the hazardous?
How Do We Diagnose Palpitations?
The most important thing when addressing patients with palpitations is to exclude underlying heart disease.
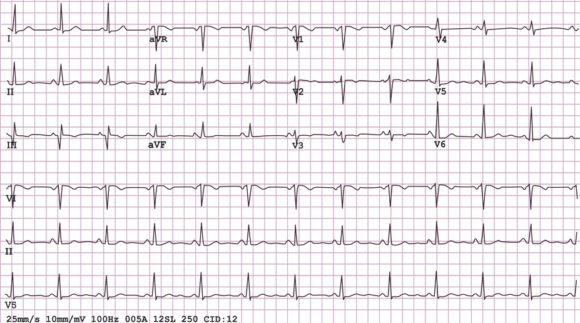
All patients should undergo a detailed history and physical examination, as well as an electrocardiogram (ECG).
However, diagnosing palpitations doesn’t start with machines—it begins with a conversation.
When a patient sits down across from me, I’m not just looking for a list of symptoms. I’m listening to how they describe what’s happening. The rhythm of their words often mirrors the rhythm they’re feeling.
I often ask questions like these:
- When do you feel the palpitations? Do they come at rest, during exertion, or in the middle of the night?
- Can you describe the feeling? Is it fast, irregular, pounding, or skipping?
- How long do they last? Seconds? Minutes?
- Are they accompanied by dizziness, shortness of breath, chest pressure, or a sense of doom?
- Do they follow coffee, alcohol, or emotional stress? What about lying down, particularly on your left side?
Interestingly, palpitations that happen when lying on the left side are often harmless. In that position, the heart nestles closer to the chest wall, making every beat more noticeable. For some, just turning over brings relief.
Once I have a sense of the story, we move to testing. Our first tool is the electrocardiogram (ECG). It’s quick, painless, and often helpful—but since palpitations can be elusive, the ECG might show nothing out of the ordinary.
Electrocardiogram (ECG)
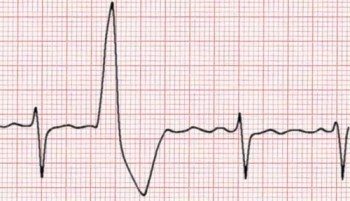
An ECG is a noninvasive test where electrodes are placed on the chest and extremities for registration of the electrical activity of the heart.
The ECG may directly detect the underlying arrhythmia causing the palpitations. However, because palpitations are usually intermittent, the ECG is most often completely normal.
In some cases, the ECG may suggest underlying heart diseases such as coronary heart disease or a thickened and strained heart muscle (left ventricular hypertrophy).
Sometimes isolated premature ventricular or supraventricular beats may be seen on the ECG, thus suggesting the underlying cause of the palpitations.
Ambulatory ECG Monitoring
When palpitations are sporadic, we use ambulatory ECG monitoring to catch them in action:
- Holter monitor: Worn for 24–72 hours; records every beat
- Event recorder: Worn longer; activated when symptoms occur
- Implantable loop recorder: Placed under the skin for long-term rhythm tracking; used for rare, unexplained cases of fainting or palpitations
And in recent years, smartphone-enabled technology has changed the game:
- Apple Watch, KardiaMobile, Withings ScanWatch, Samsung Galaxy Watch, and other devices can now record single-lead ECGs.
- Some connect directly to physician dashboards.
- Others use AI to detect patterns, such as atrial fibrillation, with remarkable accuracy.
When a patient records an episode in real time—whether it’s a short run of SVT or a benign ectopic beat—it often brings clarity. And for many, that clarity brings peace of mind.
One patient told me, “I finally caught it—the flutter I always feel—and it was just one extra beat.” In that moment, we weren’t just diagnosing a symptom. We were replacing fear with understanding.
How Are Palpitations Treated?
Treating palpitations isn’t always about medicine. Often, it begins with understanding—and the power of reassurance.
Many patients come in fearing the worst. However, after a careful evaluation, we often find that the heart is structurally fine and the rhythm is essentially normal. The palpitations are real, but not dangerous. In those moments, the best prescription isn’t a pill—it’s peace of mind.
If no underlying heart disease is found:
- Reassurance is often the most potent medicine.
- Lifestyle changes such as reducing caffeine, alcohol, and nicotine can help.
- Managing stress and anxiety is key, sometimes with help from therapy or medication.
- Addressing sleep hygiene, hydration, and diet can also make a noticeable difference.
If an arrhythmia is diagnosed:
- Beta blockers or calcium channel blockers may help reduce symptoms.
- Catheter ablation can cure certain arrhythmias, such as supraventricular tachycardia (SVT).
- Anticoagulation (blood thinners) may be necessary in atrial fibrillation to reduce stroke risk.
- Antiarrhythmic medications are used more selectively, often under the care of a specialist.
What’s the Outlook?
The good news is that the vast majority of people with palpitations have an excellent prognosis. Most arrhythmias are benign. Even when they’re annoying or frightening, they rarely point to something dangerous.
In a large study, people who sought care for palpitations had a one-year mortality of just 1.6%, and those few deaths occurred in older individuals with preexisting conditions.
That said, certain red flags warrant more attention:
- Fainting or near-fainting
- Chest pain
- Shortness of breath or dizziness
- Family history of sudden cardiac death
- Known heart disease
These flags deserve a prompt and thorough evaluation.
Final Thoughts: What I Tell My Patients
Palpitations can be unsettling, but they are not uncommon and are usually not a cause for concern.
Still, I know how real they feel. The jolt in your chest. The skipped beat that makes time stand still. The wave of uncertainty that follows.
If you’re experiencing them, don’t dismiss them—but don’t let them own you either. Begin with a calm, clear evaluation. Talk to your doctor. Wear a monitor if needed. Understand what your heart is telling you.
Many of my patients have walked into my office convinced something terrible is happening, only to walk out with relief and clarity. In most cases, palpitations are part of the body’s noisy way of adjusting to stress, fatigue, stimulants, or life itself. And once people understand the cause, they often begin to tune out the fear.
This article is a revised and updated version of one I first published a few years ago. It reflects recent clinical insights, new diagnostic tools, and a deeper understanding of how patients experience palpitations.


I suffered from palpitations for years, sometimes so bad they triggered anxiety attacks and prevented me from sleeping. I was checked out by my doctor, wore a Holter monitor, but no issues could be found.
When I adopted a ketogenic lifestyle, one of the first things I noticed, besides the immediate disappearance of the severe water retention that also plagued me, was I no longer had palpitations. So many aspects of my health improved so dramatically, that I’m not sure why they went away, but I haven’t had them since, 18 months and counting. I also noticed, as have those around me, that my general personality is much happier, so maybe the overall improvement in brain health is the cause. After my initial weight loss success, I increased my exercise, which improved my heart health even further.
I can’t recommend the lifestyle enough, it has dramatically changed our lives and our health for the better.
Very interesting. Thanks for sharing you experience.
It’s a good idea to remember that a rapid pulse can be a symptom of food allergies. I have found that my resting pulse rate goes from around 80 to around 135, after I consume soy products, especially soy protein isolate.
A question for the Doc:
Here is a link to your post on LDL-P:
https://www.docsopinion.com/health-and-nutrition/lipids/ldl-p/
What about situations where LDL-P is high, but the small LDL-P count is low? Would you focus on particle count or on particle size?
For example, some numbers from a recent LabCorp (US lab company) test:
LDL-C: 139
HDL-C: 48
Triglycerides: 138
Total Cholesterol: 215
LDL-P: 1716 (nmol/L)
HDL-P: 32.0 (umol/L), LabCorp Reference Interval, Should be > 30.5
Small LDL-P: 398 (nmol/L), LabCorp Reference Interval, Should be 20.5
(I’m note sure whether the LDL size refers to most common size, or to the average size.)
Jeffrey
Thanks for the comment.
I’m happy to respond to your comment but would prefer to do that in the comment section of the article you cited as it doesn’t really fit well here.
Will do. I wasn’t sure if you were monitoring older posts.