The authors of the paper, led by Li Yanping from the Department of Nutrition at the Harvard School of Public Health, conclude that unsaturated fatty acids, especially polyunsaturated fatty acids (PUFAs) and/or high-quality carbohydrates can be used to replace saturated fatty acids (SFAs) to reduce the risk of coronary heart disease (CHD).
Although in line with current dietary recommendations, these results contradict a systematic review and meta-analysis published last year by Chowdhury and coworkers which found no significant association between the intake of SFAs and the risk of coronary heart disease (2).
Furthermore, last February, The Scientific Report of the 2015 Dietary Guidelines Advisory Committee (DGAC) in the USA concluded that “while the body of research linking saturated fat intake to the modulation of LDL and other circulating lipoprotein concentrations is significant, this evidence is essentially irrelevant to the question of the relationship between diet and risk for cardiovascular disease (3).”
However, things tend to change rapidly (except the guidelines) in the world of nutrition science. Now, after what appeared to be a successful rehabilitation, saturated fat is back in the gutter.
But a closer look at the Yanping paper raises questions about some more obvious conclusions not addressed by the authors.
The Yanping Study
Yanping and coworkers studied combined data from the large, observational Nurses’ Health (NHS) and Health Professionals Follow-up Studies (HPFS). Approximately 127 thousand individuals free of diabetes, cardiovascular disease, and cancer were followed for 30 years. Diet was assessed by a semiquantitative food frequency questionnaire every four years.
At baseline, those who consumed the highest amount of SFAs were slightly younger, had a higher body mass index, a lower prevalence of physical activity, were more likely to be smokers, and consumed more cholesterol. They also tended to have a higher energy intake from monounsaturated fatty acids (MUFAs) and trans fats and lower energy intake from carbohydrates.
A multivariable adjusted model was used to adjust for known risk factors for coronary heart disease, including body mass index, family history of diabetes and myocardial infarction, menopausal status and hormone therapy, regular use of aspirin, smoking status, physical activity, presence of hypertension and hypercholesterolemia, and percentage of energy from protein and cholesterol.
Higher intakes of PUFAs and carbohydrates from whole grains were significantly associated with a lower risk of CHD. In contrast, carbohydrates from refined starches and added sugars were associated with higher risk of CHD. Intake of SFAs and MUFAs was not significantly associated with the risk of CHD in the multivariate model.
Replacing 5% of energy intake from SFAs with equivalent energy intake from PUFAs, MUFAs or carbohydrates from whole grains was associated with a 25%, 15% and 9% lower risk of CHD respectively. Replacing SFAs with trans fat or carbohydrates from refined starches and added sugars did not significantly affect the risk of CHD.
Interestingly, participants generally replaced calories from SFAs with calories from low-quality carbohydrates rather than calories from PUFAs or high-quality carbohydrates.
The authors conclude that their findings “provide epidemiological evidence of the current dietary guidelines, which recommend both replacing saturated fatty acids with monounsaturated and polyunsaturated fatty acids and replacing refined grains with whole grains.
They claim that consuming less SFAs will lower the risk of coronary heart disease as long as they are replaced with PUFAs or high-quality carbohydrates such as whole grains but not if they are replaced with trans fats or low-quality carbohydrates such as white bread, white rice, or potatoes.
A Closer Look at the Data
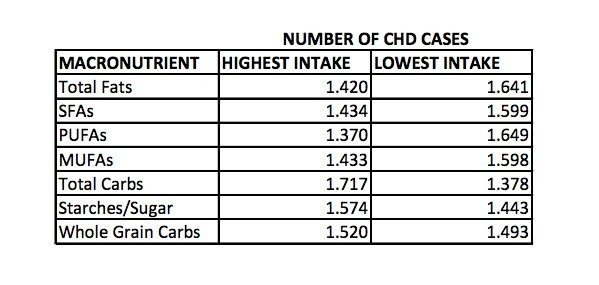
The study participants were divided into quintile categories (five groups of equal size), based on their nutritional intakes. So, for each macronutrient, there were five groups. If we take SFAs for example, the lowest quartile is the group (20% of the study population) with the lowest intake of SFAs, and the highest quartile is the group (20% of the study population) with the highest intake of SFAs.
There were 16% more cases of CHD in the group with the lowest fat intake (ca. 26% of calories) compared with the group with the highest intake (ca. 41% of calories).
Similarly, there were 12% more cases of CHD in the group with the lowest intake (ca. 9% of calories) of SFAs compared to the group with the highest intake (ca. 15% of calories).
Remember that, although slightly younger, the group who consumed most SFAs had a higher body mass index, a lower prevalence of physical activity, were more likely to be smokers, and consumed more cholesterol.
The group with the highest (ca. 56% of calories) carbohydrate consumption had 25% more cases of CHD than the group with the lowest (ca 37% of calories) carbohydrate consumption.
These numbers are not dealt with by the authors of the paper.
Saturated Fat – The Bigger Picture
Surely the study by Yanping and coworkers will encourage authors of dietary guidelines to stick with their previous recommendations highlighting restriction of SFAs and that they should be replaced with PUFAs and high-quality carbohydrates.
However, it is important to understand that, due to the study’s observational nature, it cannot prove causality. Despite the use of complex statistical methods, it is difficult to rule out confounding factors that may affect the results.
Furthermore, there are many types of SFAs with different metabolic effects and their association with CHD varies. For example, while palmitic acid appears to be associated with adverse metabolic effects, other SFAs may be associated with metabolic benefits (4).
Dietary SFAs are derived from many different foods, and these have many other ingredients and characteristics that modify their health effects. Therefore judging the health effects of foods entirely from the amount of SFAs may be dreadfully misleading.
When looking more closely at the data it appears that individuals with the highest intake of dietary fats have a lower risk of CHD than those with the lowest fat consumption.
Furthermore, those with the highest carbohydrate intake appear to have a higher risk of CHD than those with the lowest carbohydrate consumption.
Despite my deep respect for the use of statistical methods to adjust for confounding factors, I find it hard to see how statistical acrobatics might reverse this picture.
So, the numbers appear to suggest that; less fats-more heart disease, more fats-less heart disease and more carbs-more heart disease, less carbs-less heart disease. Yes, I know; correlation does not prove causation but…
I suspect the Yanping study may convince many of us that choosing PUFAs rather than SFAs and choosing whole grains rather than starches and added sugar is preferable. But what’s most important about this paper are the questions raised but regrettably left unanswered by the authors.
The lights are on, but nobody’s home.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

Damned if ya do, damned if ya don’t!
You’re more likely damned if you do. Do what? Follow the advice of the Dietary Guidelines Advisory Committee and Harvard epidemiologists to swap solvent extracted seed oils for saturated fats. (1)
The problem is, there are deleterious effects associated with high PUFA intake that have nothing to do with heart attack risk. For example: “Over recent decades, more and more of the oil in the typical American diet has come first from corn, and then from soybeans. In both cases, that oil is an unusually concentrated source of omega-6, linoleic acid. The direct metabolic implication of this is immediately clear: the production of DHA is being inhibited at an enormous scale. The public health ramifications are less clear, but clearly worrisome. Is widespread interference with the production, and brain uptake of DHA, a contributing factor to trends in autism, ADD, and other disorders of behavior and cognition? Proof of causality is an elusive standard, but the proposition is every bit as plausible as it is disturbing.” (2)
1. https://www.hsph.harvard.edu/nutritionsource/2014/11/05/dietary-linoleic-acid-and-risk-of-coronary-heart-disease/
2. https://www.huffingtonpost.com/david-katz-md/dietary-fat-and-the-human_b_8089586.html
Great article! I am a Nutrition Diagnostics Master’s student at Cox College, and this is the information that my cohort and I are just beginning to learn. It has taken my mind by storm. The “saturated fats are bad, whole grain carbohydrates are good” mantra is one that is still being taught in almost every undergraduate nutrition program in the country. It is going to be a long road ahead to try to forge these new ideas, especially with researchers suffering from growing pains. Thanks for the comprehensive report!
Thanks Leah.
I think you’re right. There’s a long road ahead.
Go for it, Leah!
Nice catch 🙂
Thanks Ashkar.
Thanks for extracting that data for us. There’s one thing I didn’t understand. The HRs for SFA and MUFA across the quintiles were almost exactly the same, with slight advantage to SFA, yet they predict benefit from replacing SFA with MUFA.
How is this possible?
George.
They perform some type of substitution analysis. The statistical approach is pretty difficult to understand; “When estimating the effect of substituting 1 type of fat or 1 source of carbohydrate for another, we included energy contributions from the 2 nutrient types as continuous variables in the same multivariable adjusted model. The differences in their coefficients and covariance were used to estimate the HR and 95% CI of the substitution.”
Still trying to figure it out 🙂
Even a stage magician needs to show there’s nothing up his sleeve. We’re not being shown that here, it has the appearance of a “proprietary formula”.
Another thing that bothers me – among many – there simply isn’t a 5%E difference between upper and lower quintile in most cases. And even if there were, a projection of benefit from the 5%E increase based on the real data could only apply to the lowest quintile.
But they’re essentially telling people in every quintile of PUFA intake to increase PUFA by 5%E.
Another issue – the exclusion criteria for plausibility of diet reporting are farcical, with 600 kcal/day being the lower cut-off.
Another – there were repeated FFQs over the study, which covered a period when fat and SFA significantly dropped, and carbohydrate increased, in the study populations.
Any attempt to aggregate this type of shifting data has to be arbitrary, and there must also be real data in there about what happened to the people who swapped nutrients that hasn’t been used.
In recent high-definition epidemiology like the Malmo Diet and Cancer study it’s possible to isolate people who changed their diet and exclude them from a model if needed.
This good quality data set shows declining CVD mortality in men with increasing fat intake (RR 0.65 in upper quartile of fat, median 47%E) , lower risk of diabetes with more SFA from dairy, and increased cancer mortality associated with high MUFA intake in women (RR 1.46 – likely associated with liquid margarine consumption as men, who ate more MUFA from meat and less from vegetable fat, had no increased cancer mortality with higher fat intake, and vegetable fat but not animal fat was associated with breast cancer in a case-control analysis).
https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2796.2005.01520.x/pdf
No effect of PUFA whatsoever in this population, quartile range was 4-8%E. This can be interpreted as meaning that when PUFA is adequate in a population, there is no benefit from an increase and no harm from a decrease.
The real problem to me is that science today in some disciplines is so poor that a person has no idea what to believe, even if one does dive into the study an tear it apart. Peer review is no panacea to fixing the system either. We know that a good portion of studies today are fraudulent or biased and as long as there’s no effort made by the journals to fix this situation I think it wise to believe that everything being published is suspect.
Because my distrust has grown so strong in the system I think my rule of thumb is a better application for the purpose of what to do in real life – if the government, dietitian or health organizations make a recommendation, do the exact opposite. It hasn’t failed me yet.
Wait a minute, There were 127,000 people in the study, followed over 30 years and there were only 7,667 that had CAD on follow-up? … that’s only 6% with CAD. Is there any real ABSOLUTE differences in the CAD risk based on diet? 25% or 9% of 6% does not move ABSOLUTE risk that much. Oh and, if the saturated fat group was younger, doesn’t that skew results (bad habits or not)? How young were these people? It looks like they are saying the optimum fat intake in % of diet is So could someone break down the correct %’s of what the heck food types I should be eating? What % of saturated fats/PUFAs, MUFAs, complex carbohydrates, whatever…… And make it come out to 100% please.
Let’s see. I went on a higher-fat (with lots of eggs), low-junk carb (grains), low-refined sugar, no-fruit juice regimen (it’s not a diet because I eat when and what I want), and dropped 20 pounds with no effort. And so have thousands of others.
And as an added benefit, I know longer take a statin.
I call Bullshit.
You may be confusing weight loss with health outcome.
Don’t they go hand-in-hand?
Not needing a statin indicates that health markers have improved, either that or that intelligence has increased.
Firstly, congrats on being off statins, that’s a great achievement.
Re my comment, simply meant that we can lose weight a number of ways…doesn’t mean it’s always healthy. You can google fellow who lost weight by just eating twinkies but prob not the best way to do it. If the weight loss you’ve experienced also works with your lipid profile then you’re on the right track, just my two cents.
Best of luck
Agree about lipid profile. Triglyceride to HDL ratio is telling and may reflect propensity for large particle LDL (a good thing). 2:1 or less is great. Dr. Haub of KSU is the twinkie guy. He also exercised like crazy and drank Muscle Milk, facts he underemphasizes. So we don’t really know what Twinkies and other junk foods contributed in his case; for his health’s sake I’m glad he didn’t go full twinkie jacket. Apart from jounalistic sensationalism there isn’t much of a case report there. We know high carb, low calorie diets can result in weight loss. Any teenager who’s invented a crazy weight loss scheme can tell you they can lose weight on junk food if they starve (I did it as a teenager on my Cream of Wheat diet–blecch). I think Dr. Haub was concerned about muscle preservation, hence exercise and Muscle Milk protein. Dr. Haub’s reported caloric intake: ~1600 Cal/day, 800 less than his prior intake.
The basic problem with the Yanping analysis and the many others of the ilk is that epidemiological dietary studies are fraught with prospects of confounding factors.
Indeed poor health outcomes and CAD risk may well be influenced by the composition of the diet. Thereore it is not wrong to study diet. But factors other than diet may also have influence. If the diet is studied to the exclusion of concern for other non-dietary influential factors then analyses and conclusions could well be misleading. There also exists a great weakness in implicating cause by association, where any causal pathway may be a process involving a number of steps. Associate alone is weak unless intermediary steps can be plausibly explained.
It ought to be borne foremost in mind that there exist a lot of physiological and endocrinological factors that must be the middle men in transposing cause (here supposed to be diet) and health outcome (in this instance CHD). This means that if dietary factors can be responsible for CHD or CAD then there must exist a plausible mechanism via which such dietary factors can ‘disturb’ or ‘disrupt’ physiological or endocrinological balance in a way that undermines prospects of health and equates to a mechanism and pathway giving rise to disease. Absence of regard for, or understanding of, intermediary steps is a great weakness in many analyses of the type here performed by Yanping & others.
There exists some further problem with the studies that are subject to analysis. The designs of the studies are rather crude. Firstly the designs are showing signs of their age. They were designed in an era when the crude work of Ancel Keys had implicated cholesterol and saturated fat in the etiology of CAD. The weaknesses in his seven countries study have been exposed time after time. And in the time that Keys studied Anitchkow and Chalatov’s write up of their positive induction of CAD in rabbits next to nobody had the means to question the merits of the results, and especially not Keys.
In 1913 Anitchkow and Chalatov added cholesterol to rabbit feed. Following sacrifice the cholesterol fed rabbits revealed evidence of the advance of atherosclerosis that the controls did not. Rabbits would not naturally eat much cholesterol as part of their wild and natural diet, but furthermore any cholesterol from the diet would not be prone to oxidation. Unfortunately the cholesterol fed to rabbit subjects under experimental conditions had been exposed to prospects of oxidation. Anitschkow, Chalatov, Keys, and everyone in the day will have thought the rabbits had been fed cholesterol. Likely they had,, but the cholesterol was contaminated, in all probability, by up to 10 alternate cholesterol oxides. It was not until 1974 that evidence emerged to suggest this, and it took well into the 1980s to begin to identify these oxy-cholesterols and establish their individual attributes.
Indeed cholesterol forms 49 alternate oxides of cholesterol, and no two have attributes that are alike. These form by alternate pathways, but isolate cholesterol to give rise to a batch, and leave such a batch exposed to air, then the progressive and time-dependent process of oxidation will begin and will give rise to around ten cholesterol oxide contaminants. The batch advances to rancid, if you like.
The seeds of Keys cholesterol and lipid hypotheses that implicated cholesterol and dietary SFAs in the etiology of CHD and CAD were sown on VERY stoney ground. Their foundations are such a nonsense that the hypotheses themselves are a nonsense. Despite this they do live on. Bullshit still baffles brains
The involvement of certain cholesterol oxides as regulatory factors in cholesterol synthesis, evidence of at least one oxy-cholesterol giving rise to necrosis of smooth muscle cells (a circumstance witness in atherosclerotic tissues), and the tireless work of Dr Kilmer McCully surrounding homocysteine, do all, quite rationally, implicate some form of oxidative stress as being a plausible pathway and mechanism in the etiology of CAD. What’s more is that oxidative stress can be discussed in terms that link it with physiological imbalance and endocrionolgical disturbance. ‘Environmental’ stress can give rise to physiological stress – stress that equates to oxidative stress. Emotional stress, work related stress, and a poor diet, and poor lifestyle choices, can undermine the workings of the physiology, disturb the endocrinology, and add to the attrition cause by oxidative stress.
Speaking quite rationally, and with feet frimly planted with regard for the significance of evolution to biology and biochemistry, saturated fat (SFAs) is an old-fashioned component in the food chain, and an old-fashioned food for humans.
On the other hand refined ‘white’ carbohydrates present in the human diet in quantity represents a more modern phenomenon. Likewise the supply of PUFAs presnt in the diet today contrasts with diets of the past. The omega-6 varieties are now more likely to be present in greater quantity since these stem, potentially in bulk, from the growing of oil-seed crops to be milled, refined, and sold on to the public as cooking oils and margarine. Old-fashioned foods these are not.
If I wanted to hunt down suspects of old-fashioned diseases I would look to old-fashioned phenomena. Cholera, for instance can be promoted by high density living and old-fashioned inadequate provision to deal with sewerage.
Conversely if I had to turn detective to try to establish the cause of a modern disease then I would turn attention to modern phenomena first and old-fashioned phenomena last. Barry Groves did this at length and implied diets high in refined ‘white’ carbohydrates allied to diets high in refined PUFAs (omega-6) originating from the milling of seed-oil crops could be associated with a series of disease of the degenerative type.
And while the balance of the diet can contribute to the process of oxidative stress, and while a poor diet can be deficient in the amount of defensive and health promoting antioxidants it can supply, Things such as stress, light stress, and the stress associating with a paucity of supply of free-electrons from ground (aggravated by the extent to which man-made materials feature in modern footwear), also feed into physiological and endocrinological stress – stress of an oxidative kind.
So, now presented with a thumbnail sketch of the mechanism(s) that feed the etiology of disease, with emphasis in this case upon CHD, it is possible to begin to see clearly just how primitive designs of studies, such as the Nurses Health Study, whose data gathering methods relied upon a semi-quantitative food frequency questionnaire to be completes every four years, are. If the design is crude the data will be crude. Then if the data is crude no amount of analysis will amount to sophisticated analysis, irrespective of how polished it may appear. If the analysts have coprolite then now amount of polishing will result in anything other than a polished, but still crude, coprolite. (A coprolite is a fossilised turd – for those who might not know.)
People interested in studying the etiology of generative diseases whose case histories, predominantly, cannot fit the generally rigorous description of being congenital by nature, would do well to learn that species that eat food and metabolise it in the presence cannot avoid oxidative stress. The physiology of such species provide many and sophiticated mechanisms for the management of oxidative stress. An enzyme (or enzymes) given over to the processing of the highly radical hydrogen peroxide being one example. Supply of antioxidants from diet being other examples, allied to four alternate prominent antioxidant pathways. Methylation being one.
Oxidation stress is the ticking of your biological clock. Your time alive is always going to run out. How fast your time runs out will be a function, primarily, of how must oxidative stress the body is exposed to as life advances with the clock ticking all the while. The second degree of function in determining how soon the bilogical clock must stop ticking is about a delicate and important balance, this being the measure of exposure to oxidation stress versus the supply the balance of supply of those all important and defensive antioxidants. Now we can begin to see that the composition of the diet might impair this balance, there may exists disproportionate oxidatve stress and too few antioxidants associating with the dietary composition. But crucially factors other than diet also have bearing upon this balance. These ‘other factors’ need not confound us, but where the design of studies like the NHS, the HPFS, the ‘Framingham’, and others of their ilk are concerned, the designs are so limited in scope and sophistication that amount to confounding factors. They have been contraversial, and far from adequately conclusive.
Joined-up-thinking isn’t easy in the absence of an appreciation of the scope of the things that must be joined. But joined-up-thinking becomes a little easier once one becomes more aware of the factors that need joining. In the least Yanping begins with a fixation that others established before, but which places an emphasis upon too few factors, factors that are not wheel recorded by the design, and therefore cannot stand as truly wholesome data, and that distract the mind from unseen factors that are as significant in the mix, if not more so. We have listened to the idiots, without thought, for far too long. We can do joined-up thinking for ourselves. We just have to start thinking – critically. My only qualification to speak of is vocational driving licence – if I can do it anyone can.
Pointers for the interested and those devoted to open-mindedness:
Book: Trick and Treat; Barry Groves.
Book: Earthing; Ober, Sinatra, & Zucker.
Book: Lights Out; Wiley & Formby.
Book: Biological Effects of Cholesterol Oxides; Peng & Morin (as contr eds.)
Book: Diet Delusion; Gary Taubes.
Book: The Forth Phase of Water: Gerald Pollack.
Interesting thing about the cholesterol-fed rabbit model of CAD is that MUFA often comes off worse than SFA, and butter high in CLA is protective, as are choline and chondroitin.
What’s truly interesting is people who talk about animal feeding studies when we have ample evidence from human studies (metabolic ward) of the effects of fatty acids.
Less SAFA & sugar/junk carbs –> better health. Simplified, yes, but still valid.
Could you cite a study where they reduced saturated fatty acids and that resulted in lower heart disease (or “better health” in any way)?
In the meantime, here’s my study: The women’s health initiative (diet arm), where they took 59,000 women and randomized them into two groups. One group was actively counseled to eat less overall fat, less saturated fat, more fruits and vegetables, etc., and they did (and reduced that “evil” red meat too, by a statistically significant amount). After 8 years and half a billion dollars, there was no statistically significant difference between the two groups in heart disease, cancer, even weight (one pound). This is the largest randomized controlled trial ever done. To me, that ends the debate over saturated fat and the low fat diet.
If you need another study, look at MRFIT. Yet another failure.
“Could you cite a study where they reduced saturated fatty acids and that resulted in lower heart disease (or “better health” in any way)?”
If by “reduced” you mean “exchanged safa for pufa”, then e.g. LA Veterans. Mere reduction means nothing because the calories still come from somewhere – and that “somewhere” is the key here. Safa –> Western carbs = not a good idea.
About WHI: the study goes to show that people cannot make the required changes and/or that the changes they make aren’t what they should be (e.g. reducing total fat isn’t the way to go). What you failed to mention was that while the changes were statistically significant, they weren’t CLINICALLY significant (e.g. LDL levels were virtually the same).
Therefore, WHI can be used to argue for nothing more than the inadequacy of dietary changes alone. It certainly doesn’t show (unlike you’re implying) that exchanging safa for pufa/low GI carbs is useless: the study couldn’t even address that!
Axel, you stated:
“I suspect the Yanping study may convince many of us that choosing PUFAs rather than SFAs and choosing whole grains rather than starches and added sugar is preferable.”
The wording is a bit funny/awkward. Did you mean to imply that you have a problem with this recommendation?
BTW, I find it … somewhat disingenuous that you continue referring to Chowdbury et al without acknowledging the problems inherent in it. Why do you allow comments here if you choose to ignore/not to reply the points made by the commenters?
Thanks for the comment MIe.
No, I don’t have a problem with the “choosing PUFAs rather than SFAs” recommendation. I think it’s valid for individuals with atherosclerotic heart disease and as a general recommendation. However, I don’t think it’s of key importance, to some extent misleading, and that we should focus on foods rather than macronutrients.
Many (most) systematic reviews have inherent problems and I don’t doubt that Chowdhury’s one of them. However, they can still be cited or referred to.
Finally, I never ignore comments, but due to lack of time I’m not able to respond to all of them.
“However, I don’t think it’s of key importance, to some extent misleading, and that we should focus on foods rather than macronutrients.”
Could you clarify the first two a bit, please? I agree with on the third one.
(… which is, BTW, precisely the direction where the current recommendations – at least Nordic/Finnish guidelines – have been heading for quite some time. However, if you focus on entire foods – or better yet, DIETS – you more or less end up in a situation where both SAFA and sugar intake get minimized.)
“Many (most) systematic reviews have inherent problems and I don’t doubt that Chowdhury’s one of them. However, they can still be cited or referred to.”
Of course, if you wish to ignore the problems this causes.
“Finally, I never ignore comments, but due to lack of time I’m not able to respond to all of them.”
So you choose not to respond to those that are most challenging? 🙂
Mie.
I believe the evidence suggesting replacing SFAs with PUFAs is weak which is one of the reason I don’t consider this recommendation to be of key importance. Furthermore, PUFAs are heterogenous. Some, like EPA and DHA may have more benefits than other. SFA’s are also heterogenous, some appear to have positive beneficial effects while others don’t. This is one of the reasons I use the word misleading.
The evidence that SFAs lower triglyceride-rich lipoproteins and lipoprotein(a), and the lack of evidence for a relationship between SFA intake and coronary heart disease, and no proven harm for most major food sources containing SFAs, don’t suggest that SFAs per se are harmful.
“I believe the evidence suggesting replacing SFAs with PUFAs is weak ”
And yet you continue to utter statements which are much less supported by evidence than the abovementioned (e.g. in this very message of yours). Selective, at best.
“Furthermore, PUFAs are heterogenous. Some, like EPA and DHA may have more benefits than others.”
… which (heterogenuity) is a moot point as there’s evidence of both n-3 and n-6 fatty acids being beneficial when consumed within intakes recommended in (virtually all) the guidelines.
“SFAs are also heterogenous, some appear to have beneficial metabolic effects while others don’t.”
You’re referring to the EPIC study you referenced? Err, there’s a) trial evidence indicating that some of the SAFA’s listed as indicating benefits in DM2 are anything but cardioprotective and b) all the others (if I recall correctly) are from dairy products, which I’d consider confounding as the benefits of dairy products seem to be independent of their fat.
“The evidence that SFAs lower triglyceride-rich lipoproteins and lipoprotein(a), and the lack of evidence for a relationship between SFA intake and coronary heart disease, and no proven harm for most major food sources containing SFAs, don’t suggest that SFAs per se are harmful.”
1) Axel, both MUFA and PUFA lower triglycerides, too (PUFA has the strongest effect) – in addition to LDL & ApoB lowering etc. etc. where SAFA has no effect or a deleterious effect. And SAFA actually increases Apo-A, see e.g. Mensink et al (2003). So no reasons for increasing SAFA intake there, nope.
2) As for the “lack of evidence”, you mean the Chowdbury et al with numerous problems, all of which I’ve mentioned before – several times, BTW?
3) And there’s no “proven harm” (in other words, no benefit/downsides over junk carbs) of e.g. butter, red meat etc. etc. in comparison to e.g. nuts, fish etc. etc., eh?? 🙂
Thanks Mie.
Don’t know what I’d do without you 🙂
But, I never said that we should increase SFA intake.
And, I always try to choose fish, nuts, vegetables and olive oil rather than processed meat and junk carbs, I think everybody should. But, I don’t think it has anything to do with the amount of saturated fats. There are other measures to assess whether a food is healthy or not. And I love some butter and cream in between.
By the way. Do you believe that all studies that don’t support your opinion are flawed?
And I think his name is Chowdhury, not Chowdbury.
“Thanks Mie. Don’t know what I’d do without you :)”
Ignore the key points in someone else’s posts?
How about you try a little something called “argumentation”? 🙂
“But, I never said that we should increase SFA intake.”
If SAFA is harmless – as you claim – why shouldn’t we? If there’s next to no evidence for the benefits of fat exchange – as you claim – why shouldn’t we? Or how about you define “key importance”: does fat exchange (SAFA for PUFA) matter or not?
“And, I always try to choose fish, nuts, vegetables and olive oil rather than processed meat and junk carbs, I think everybody should. But, I don’t think it has anything to do with saturated fats.”
Well, not if you consider junk carbs (mopstly sugar), of course. But if the differences in e.g. red meat aren’t about fat at all, then what? We all know that there are other factors in play, but that was never my point.
“By the way. Do you believe that most studies that don’t support your opinion are flawed?”
Nope. If there’s evidence for it, I’ll change my opinion.
For your information, I actually kinda bought that SAFA-whitewash nonsense for a while. Then I read the meta-analyses and the original studies in detail. You seem to have gone in the opposite direction even though these recent meta-analyses have actually added nothing: trial evidence is still in many ways confounded due to problems inherent in trials (for instance, people don’t follow the instructions –> no real differences in SAFA intake between groups/they exchange SAFA for junk carbs/cut down on total fat intake etc. etc.) and cohort studies in general haven’t inspected what people replaced SAFA with.
“And I think the name of the guy who wrote the “numerous problems” paper is Chowdhury, not Chowdbury.”
Typo, my bad.
https://money.cnn.com/2015/10/26/news/red-meat-processed-cancer-world-health-organization/
Meat bad, Vegetable good. Gorg not eat dinosaur any more… eat green stuff.
From years of trial and error I have determined that I do far better on a low saturated fat diet. This article won’t change my mind one iota.
https://sverigesradio.se/sida/artikel.aspx?programid=2054&artikel=5606616
That was 2013. So was this https://www.docsopinion.com/2013/08/04/accused-of-a-crime-that-never-happened-lchf-on-trial/
Is cheese a good source of saturated fats?
Correct, I have watched Harvard Medical go down the tube … with many doctors being paid by BigPharma and BigSugar, just really hard to get info, but some is coming out. … and this is no diff, as I do not believe much of what comes out of Harvard anymore.
There is much more positive evidence coming out of LCHF dieting, since “There is NO known Carbohydrate Deficiency Disease”, and no proof that we need any carbs.
70 Going On 100