Estimated reading time: 6 minutes
Recent scientific evidence shows that the blood concentration of lipoprotein(a) (Lp(a)) is an important marker for the risk of developing heart disease. Nonetheless, Lp(a) measurements are not widely available and are seldom used in routine clinical practice.
A traditional lipid panel measures total cholesterol, triglycerides,and high-density lipoprotein cholesterol (HDL-C) The numbers are then used to calculate low-density lipoprotein cholesterol (LDL-C), which is strongly correlated with the risk of coronary heart disease and stroke.
Lately, measuring the concentration or number of lipoprotein particles has been found to be useful to assess risk. Examples of such measurements are measurements of LDL particle number (LDL-P), apolipoprotein B and Lp(a).
It has been known for some time that Lp(a) is a decisive risk factor for developing coronary heart disease and calcific narrowing of the aortic valve (aortic valve stenosis). However, the lack of clinical trial data has caused it to be largely ignored by the medical community. This is mainly due to the absence of lifestyle measures or therapies that may lower blood levels of Lp(a).
Blood levels of Lp(a) are genetically determined, meaning that environmental factors have a limited influence on the blood levels of the substance.
What Is Lipoprotein(a)?
Lipoproteins are particles that transport cholesterol and triglycerides in the bloodstream. They are composed of proteins (apolipoproteins), phospholipids, triglycerides, and cholesterol.
The lipoproteins vary in the major lipoprotein present and the relative contents of the different lipid components.
There are six major types of lipoproteins; chylomicrons, very-low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and Lp(a)
Lp(a) was first described by Kåre Berg, a Norwegian professor, in 1963 (1). It is a type of low-density lipoprotein and is rich in cholesterol.
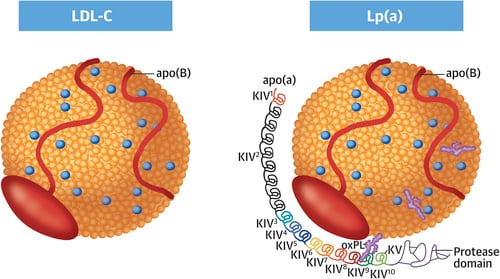
Lp(a)consists of an LDL-like core lipoprotein molecule but differs from other lipoproteins as it contains a unique apolipoprotein(a) or apo(a)(2).
Similar to LDL, an Lp(a) particle also contains one molecule of apolipoprotein B (apoB).
Lipoproteins that promote atherosclerosis (the leading underlying cause of heart disease) are termed atherogenic. ApoB is an essential component of all atherogenic lipoproteins.
How Does an Excess of Lipoprotein(a) Cause Heart Disease?
There are several mechanisms by which Lp(a) may cause heart disease.
Firstly, like all other Apo B containing lipoproteins, Lp(a) may enter the arterial wall and promote inflammatory reactions, subsequently leading to atherosclerosis (3).
Secondly, Lp(a) is an important carrier of oxidized phospholipids (OxPLs) (4).
Blood levels of OxPLs have been previously demonstrated to be strongly associated with atherosclerotic cardiovascular disease (5). Furthermore, OxPLs seem to be associated with an increased risk of developing calcified aortic valve stenosis (6).
Thirdly, the apolioprotein (a) component of Lp(a) resembles plasminogen, an important enzyme participating in the dissolution of blood clots. Therefore, it has been suggested that high levels of Lp(a) may inhibit the natural role of plasminogen and thereby increase the risk of blood clots (7).
Lipoprotein(a) and Coronary Heart Disease
Several studies have shown that Lp(a) is a significant risk factor for developing coronary heart disease.
In a summary of 36 cohort studies, Lp(a) levels were found to be associated with increased risk of coronary heart disease and stroke (8).
In the Copenhagen City Heart Study, elevated Lp(a) levels were associated with a 1.9- and 2.6-fold increased risk of myocardial infarction (heart attack) over a 16-year follow-up period (9).
Mendelian randomization studies have provided strong evidence for a direct causative role of Lp(a) in the development of coronary heart disease (10, 11, 12).
A recently published case-control study predicted that pharmacologic reduction of Lp(a) in individuals with the highest concentration would substantially decrease the risk of cardiovascular disease (13).
Lipoprotein(a) and Aortic Valve Stenosis
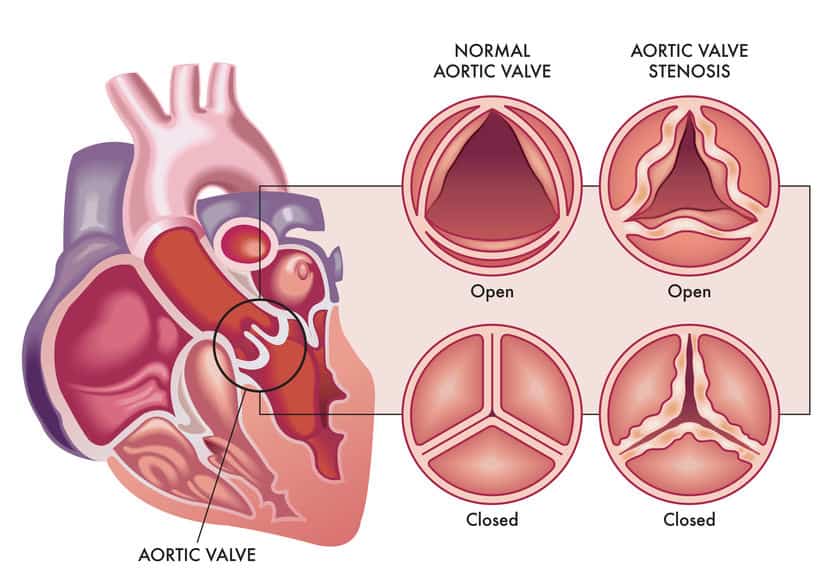
Aortic valve abnormalities are pretty frequent in older people. A thickening or calcification of the aortic valve or calcification, without significant obstruction, is found in 26 percent of people older than 65 years (14).
In some people, the aortic valve’s leaflets may become stiff, leading to a narrowing of the aortic valve opening. If severe, this may obstruct blood flow from the left ventricle; a condition called aortic valve stenosis.
Clinical studies demonstrate a significant association between Lp(a) levels and aortic valve stenosis.
Furthermore, genome-wide and Mendelian randomization studies suggest that high Lp(a) levels play a causative role in developing the disorder (4).
What Is the Normal Range For Blood Levels of Lipoprotein(a)?
Here’s how Lp(a) levels are looked at in terms of risk:
- Desirable: < 14 mg/dL (< 35 nmol/l)
- Borderline risk: 14 – 30 mg/dL (35 – 75 nmol/l)
- High risk: 31 – 50 mg/dL (75 – 125 nmol/l)
- Very high risk: > 50 mg/dL (> 125 nmol/l)
How Can Lipoprotein(a) Be Modulated?
Lp(a) levels are primarily genetically determined. Nonetheless, lifestyle factors may also play a role.
Studies on the effect of diet on Lp(a) levels are limited. However, low-fat diets, in particular, seem to result in a small but significant increase in Lp(a)(15,16)
Interestingly, a low-fat, high-carbohydrate diet may increase Lp(a) levels compared to a high-fat, low-carbohydrate diet (16).
The data on the effect of statin drugs on Lp(a)levels are conflicting.
For example, one study showed that statins significantly increase plasma Lp(a) levels (17). However, the same study suggested that statins lowered non-HDL cholesterol substantially and reduced overall cardiovascular risk.
Niacin decreases Lp(a) levels by approximately 20%-30% (18).
PCSK9 inhibitors lower Lp(a) by approximately 20%-30% (4).
Recently, Lp(a)-specific lowering medications have become available. Major ongoing clinical trials are investigating the clinical efficacy of these agents in patients with elevated Lp(a) levels.
The HORIZON phase III trial is investigating the benefit of Lp(a)-lowering with an antisense oligonucleotide (ASO), TQJ230, compared to placebo, on major cardiovascular events, in patients with established cardiovascular disease (19).
The Take-Home Message
Lipoprotein(a) is a strong risk factor for developing coronary heart disease and calcific narrowing of the aortic valve (aortic valve stenosis).
Mendelian randomization studies have provided strong evidence for a direct causative role of Lipoprotein(a) in developing these disorders.
Lipoprotein(a) levels are primarily genetically determined. Nonetheless, lifestyle factors may also play a role.
High-fat, low-carbohydrate diets lower lipoprotein(a) more effectively than low-fat diets.
Major ongoing clinical trials are currently investigating the clinical efficacy of specific lipoprotein(a)-lowering agents in patients with elevated lipoprotein(a) levels.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

How Lpa may enter the arterial wall?
Hi Gilles
It probably enters the vessel wall in a similar manner that LDL does: https://www.docsopinion.com/low-density-lipoprotein-atherosclerosis-heart-disease/
mine is <15, but I have a 362 CAC score, so it didn't help me any to have a low LP(a)
Hi Michael
I’m not sure I agree.
In theory, your coronary calcium score might have been higher than 362 if your Lp(a) was elevated.
And, of course, many other factors are involved in the calcification of the coronary arteries.
I’ve been getting my Lp(a) tested over the course of the last 8 years (went low carb/keto on 1/1/14), and my Lp(a) is ridiculously high over that time, between 220-360+ mmol/l, yet I got a zero score on CAC at about 5.5 year point. 90% of people had higher CAC scores (I was 55 at the time).
I also have no aortic stenosis, as verified by multiple transthoracic echocardiograms over that period.
Finally, I believe PUFAs cause higher values of Lp(a) and saturated fat can lower these values. I’m in the process of setting up a test of this to verify, though whether I can afford the costs of the multiple blood tests will be a factor as to whether I can do the actual test.
interesting, dr. sigurdsson, no lab report has included lp(a). everything else it seems is there!
Lp(a) is due because the human body cannot produce vitamin C. As a result Lp(a) is the patchwork necessary when micro tears occur within the arterial wall (i.e. endothelium aka glycocalyx). This is well documented by the research done by Drs. Rath & Pauling.
Dr. Rath concluded that sufficient amounts of L-Pro and L-Lys would in effect remove the Lp(a) residue. This in conjunction with mega-dosing Vit. C would far exceed niacin therapy or PCSK9 both of which only reduce 20-30 % Lp(a). B3 over time raises FBS, PCSK9s have been reported to cause ‘neurocognitive effects’ (attention deficit and confusion) and Antisense Oligonucleotides have an FDA Warning label for hepato-toxcicity, elevated serum transaminase, and hepatic steatosis
Thanks Doc! Particularly relevant to both myself and family. My father recently had a TAVI due to AO. A background in endurance sports (Int. level) and still riding at 82yrs with very clear coronary arteries. We have near identical cholesterol profiles and I’ve been logging miles most of my life. A recent echo showed no stenosis but it’s on my radar and won’t be unexpected. Keep writing!
Speaking of entering the arterial wall, a research paper from the Salk Institute a couple of months ago seems to show that the spike protein used by Covid to enter cells and released/created? by mRNA vaccines may cause vascular damage.
=========
Salk researchers and collaborators show how the protein damages cells, confirming COVID-19 as a primarily vascular disease
April 30, 2021
https://www.salk.edu/news-release/the-novel-coronavirus-spike-protein-plays-additional-key-role-in-illness/
===========
Do you have any thoughts on this aspect of Covid & related mRNA vaccines?
I just received my full lipid panel after my dad passed away from atherosclerosis. My total cholesterol is 214, HDL 62, LDL-C 135, non-HDL 152, LDL-P 1,474, Apolipoprotein B 105, Lipoprotein 206, trigylcerides 71. I’m only 33, do not have high blood pressure or diabetes, but am slightly overweight. I’m not sure if I should be concerned or not, but given the circumstances with my dad recently passing, I’m scared. Should I be on medication or is this something I can correct with lifestyle modifications?
Yes I would be concerned. While you are still young you can control your high cholesterol levels by eating healthy and exercising regularly. However if you are not able to significantly reduce these mentioned cholesterol levels in another 6 months then you should be on low dose statins ( prescribed cholesterol lowering drugs)
So if you have a score of 9 nmol / L (lab ref value <75) for Lp(a) and HDL of 58, Triglycerides of 62, Total of 186 and LDL of 114 and hs-CRP of .45, yet have a CAC score of 385 in the LAD and 0 in two other arteries and 50 in the remaining one. Particle number 1164 (down from 1450 7 years prior), small LDL-P 202 nmol/L (lab ref 20.5). 70 years old with type 1.5 diabetes (20+years)rheumatoid arthritis of 20+ years (in remission with Enbrel for past 8 years). HBA1c of 5.8.
Eat 20% carbs, 25% protein, 55% fat. Walk 5 miles/day at 4mph pace – semi-hilly terrain. Heart rate gets up to 135 at peak of walk. No difficulties with breathing or chest pain.
What do you make of the CAC score and what to do about it based on my numbers and info above? Docs all want me on statins. Have declined this option due to having too many friends with serious issues from them. I am trying to eat a low inflammatory diet with high doses of fish oil, 1-2 grams of Kyolic Aged Garlic Extract, CoQ10 (200mg/day), multi-Vit, Quercetin, Circumin, folate,Vit D 5000IU,400-600mg of chelated Magnesium, Collagen powder. Thinking about taking d-ribose and l-carnitine per Dr Stephan Sinatra theory of providing additional energy to the heart.
Thanks for any thoughts you might have!
Mark
56 year old Male, CAC 12.9, 12 of that in Right coronary. TC 209, LDL 138, Trig 122, but I have high bp, especially in AM upon waking, varies wildly, e.g. 160/101 ten minutes after waking, down to 127/78 one hour later. Trying to fix diet, not easy.
Some Centenarians have elevated levels of Lipoprotein (a) so it might be protective or a good thing as it’s in the genetics for a reason.
https://pubmed.ncbi.nlm.nih.gov/9543111/
https://pubmed.ncbi.nlm.nih.gov/9535215/
I have a calcium score of about 3500
Had a double bypass January due to severely calcified blocked coronary veins
And have lp(a) level of 839 mg/l
What is my prognosis and can I do something to improve this besides healthy food and daily sport/ training what I am already doing
I use ezetimibe because cannot use statins due to muscle/ boneproblems
Axel, I am writing a paper on Lp(a) and would like to use your diagram of the LDL and Lp(a) particles if that is possible.
Thanks for a good article!
Hi Allen
That’s fine as far as I´m concerned.
Good luck with your paper.
Axel
Hi, could I use you LDL/Lp(a) image for a presentation? In this case, a picture is worth a thousand words, and I feel like your image is doing a particularly good job.
Thank you