Estimated reading time: 16 minutes
The term angina pectoris or angina is used to describe chest pain or discomfort, often felt like pressure or a squeezing sensation in the chest. The pain may radiate to the shoulders, arms, neck, jaw or the back region between the shoulder blades.
Angina is not a disease. It is a symptom, usually caused by inadequate blood flow in a coronary artery resulting in insufficient supply of oxygen-rich blood to an area of the heart muscle. Hence, in most cases, angina reflects underlying coronary artery disease.
![]()
In most patients with chest pain, it is related to other, usually less severe disorders, such as musculoskeletal, gastroesophageal or anxiety syndromes. However, data show that failure to diagnose coronary artery disease is a common cause of malpractice awards against emergency medicine physicians in the United States (1).
Nowadays, all chest pain is regarded as suspected coronary artery disease until proven otherwise. Most emergency departments have chest pain units, a fast track service for patients with chest pain, relying to a large extent on blood testing, electrocardiogram, exercise testing and imaging techniques. The objectives of the chest pain units are to triage high-risk patients into fast-track therapy and to recognize low-risk patients for assignment to more careful evaluation and treatment (2).
In an era where speed has become such an important target and technology drives our conclusions and decisions, it may be justifiable to unfold the original description of angina pectoris.
The First Description of Angina Pectoris
Willam Heberden (1710-1801) was a highly regarded physician who practiced in London in the 18th century after having been a fellow of St. John’s College in Cambridge for a some years. He presented his remarkably explicit and almost lyrical description of angina pectoris at the Royal College of Physicians in London in 1768 (3).
There is a disorder of the breast, marked with strong and peculiar symptoms, considerable for the kind of danger belonging to it, and not extremely rare, of which I do not recollect any mention among medical authors. The seat of it, and sense of strangling and anxiety with which it is attended, may make it not improperly be called angina pectoris. Those who are afflicted with it are seized, while they are walking, and more particularly when they walk soon after eating, with a painful and most disagreeable sensation in the breast, which seems as if it would take their life away, if it were to increase or to continue: the moment they stand still, all this uneasiness vanishes. In all other respects the patients are at the beginning of this disorder perfectly well, and in particular have no shortness of breath, from which it is totally different. After it has continued some months, it will not cease instantaneously by standing still; and it will come on, not only when the persons are walking, but when they are lying down and oblige them to rise up out of their beds every night for many months together.
Clearly, Heberden was well aware of the strangling or squeezing sensation in the chest as well as the sense of unease or anxiety that is felt by so many patients with angina pectoris. The association with physical effort is also very clear and so is the fact that many patients experience angina after consuming a heavy meal. Heberden also acknowledged the progressive nature of the disorder and that ultimately many patients may experience angina even while resting.
Interestingly, Heberden never implied that angina pectoris reflected an underlying disease of the heart or the arteries. Because pulse was usually normal during an attack, he discounted the possibility that angina was caused by some cardiac condition (4). However, Heberden was well aware of the risks associated with the disorder. He clearly understood that angina was associated with increased risk of sudden death. He wrote:
The termination of the angina pectoris is remarkable. For if no accident interferes, but the disease goes on to its height, the patients all suddenly fall down, and perish almost immediately. Of which indeed their frequent faintness and sensations as if all the powers of life were failing, afford no obscure intimation.
It was Heberden’s friend, Edward Jenner (1749–1823) who first suggested in 1786, after observing an autopsy of a patient who had suffered from angina, that the disorder might have something to do with a disease of the coronary arteries.
Coronary Artery Disease
The role of the left ventricle of the heart is to pump oxygen-rich blood through the arteries providing oxygen and nutrition to all tissues and organs in the body. Without oxygen, glucose and other nutrients, cells will die, and if oxygen supply is limited, healthy cellular metabolism will soon be affected.
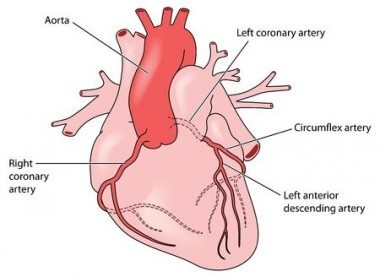
The heart muscle also needs its own blood supply to be able to thrive. The coronary arteries provide arterial blood supply to the left ventricular muscle. Two major coronary arteries, the left and the right coronary artery, branch off from the aorta near the point where the aorta and the left ventricle meet.
Atherosclerosis, the underlying cause of coronary heart disease is characterized by an accumulation of lipids, white blood cells, and cell debris in the inner layers of the arterial wall (5).
The coronary arteries are commonly affected by atherosclerosis. Atherosclerotic plaques may block blood flow in these arteries, causing ischemia and infarction.
Myocardial Ischemia and Angina
Ischemia is a result of inadequate blood flow to an organ or tissue. Myocardium is a term used for heart muscle. Hence, myocardial ischemia describes a condition of the heart muscle where arterial blood flow is inadequate.
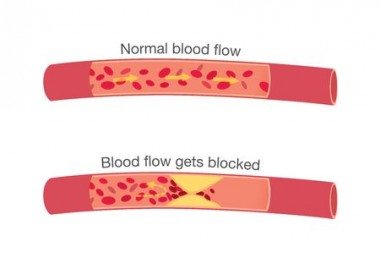
Myocardial ischemia, and consequently angina, occurs whenever myocardial oxygen demand exceeds oxygen supply. Usually, this is due to narrowing or blockage to blood flow in coronary artery resulting from atherosclerosis.
Typically, a patient with angina will experience no symptoms at rest. However, during exercise myocardial oxygen demands will increase because more energy is needed. If blood supply in a coronary artery is limited, oxygen requirements will exceed oxygen supply and myocardial ischemia will occur causing chest pain typical of angina. If the patient stops exercising, oxygen supply will again meet demands, and angina will resolve.
Myocardial Infarction and the Vulnerable Plaque
Some atherosclerotic plaques are prone to rupture. Plaque rupture is one of the most feared complications of coronary artery disease because it may lead to an abrupt occlusion of the vessel causing myocardial infarction and sometimes sudden death (6).
Infarction is irreversible damage to cells and tissue, usually resulting from an abrupt occlusion of the supplying vessel, causing local death of the tissue. The main difference between ischemia and infarction is that the former is reversible while the latter is not. Thus, myocardial infarction describes an irreversible damage to the heart muscle. A heart attack is the layman term for myocardial infarction.
Atherosclerotic plaques may become large over time and bulge into the lumen of a coronary artery, limiting blood flow to the myocardium, sometimes causing angina. However, these plaques are not necessarily prone to rupture because the risk of plaque rupture depends on plaque type (composition) rather than plaque size (volume). An atherosclerotic plaque that is prone to rupture is defined as a vulnerable plaque whereas a plaque that is not prone to rupture is considered a stable plaque.
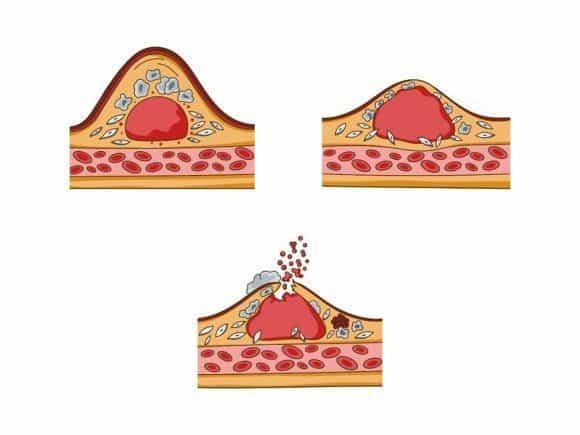
A vulnerable plaque is characterized by a thin fibrous cap, large lipid-rich necrotic core, and plaque inflammation (7).
Rupture of the plaque surface, often with superimposed blood clotting (thrombosis), frequently occurs during the evolution of coronary atherosclerotic lesions. It is an important mechanism underlying most cases of acute heart attack and sudden cardiac death (8).
One of the greatest challenges facing atherosclerotic research is identifying how and why plaques become vulnerable and how this may be translated into clinical practice. Currently available vascular imaging techniques have a limited ability to assess plaque morphology and vulnerability.
Stable vs. Unstable Angina
The type of angina pectoris so well defined by William Heberden more than 250 years ago is by definition a stable disease, basically implying that there is no immediate danger to the patient. The clinical picture is often defined as stable angina or chronic angina (9).
Unstable angina is a term that is used to describe a new onset of angina or a change in a previously stable pattern. Hence, it would apply to a patient describing a recent onset of chest pain typical of angina or someone with a history of angina experiencing increasing discomfort or symptoms at rest.
Unstable angina belongs to a spectrum of clinical presentations referred to collectively as acute coronary syndromes (ACS). It covers a range of conditions associated with sudden, reduced blood flow to the heart. The syndrome also includes conditions such as ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) (10). The underlying mechanism usually involves the rupture of an atherosclerotic plaque. Unstable angina should be treated as an emergency.
Other Causes of Angina
Because myocardial ischemia occurs whenever myocardial oxygen demand exceeds oxygen supply, angina may be the result of limited blood supply, increased demand, or both.
Coronary artery disease resulting from atherosclerotic plaques is by far the most common cause of limited blood supply to the heart muscle. However, there may be other underlying causes of limited oxygen supply to the myocardium. For example, patients with anemia may experience angina because there are not enough red blood cells to carry oxygen in the blood (11).
Variant angina (Prinzmetal angina) is caused by spasm in a coronary artery resulting in limited blood flow and myocardial ischemia (12). It usually occurs while at rest, most commonly between midnight and early morning, and the pain can be severe.
Patients with valvular disorders such as aortic valve stenosis may experience angina despite normal coronary arteries (13). The valvular stenosis leads to a thickening (hypertrophy) of the left ventricle thereby increasing oxygen demands resulting in angina (14).
Diagnosis
The first approach when evaluating patients with chest pain is to identify those at high risk (e.g., patients with acute coronary syndrome) because they will need immediate care.
History plays a critical role. The character of the chest pain (burning, constricting, dull, sharp squeezing, etc.) can help differentiate between cardiac, respiratory, gastroesophageal, musculoskeletal and other causes.
The severity, location, and duration of the pain should be outlined. Pain that radiates to the jaw or arms may suggest angina. Are there any exacerbating or relieving factors? Is the pain worsened during inspiration? Angina is more likely to be brought on by exercise or emotion. Pain brought on by food, lying down, hot drinks, or alcohol, and relieved by antacids suggests a gastrointestinal cause.

Past medical history is also important. The presence of risk factors such as family history, smoking, lipid abnormalities, overweight or obesity, diabetes, and high blood pressure support a cardiac cause.
However, in most cases, clinical presentation alone cannot reliably determine the cause of chest pain. Several diagnostic tests are available to determine the presence and severity of underlying coronary artery disease. Examples are: electrocardiogram (ECG), exercise stress testing, stress echocardiography (15), radionuclide myocardial perfusion imaging (MPI)(16), cardiac magnetic resonance (CMR)(17), coronary computed tomography angiography (CCTA)(18), and invasive coronary angiography (cardiac catheterization) (19).
Treatment
There are two primary goals for the treatment of angina pectoris. Firstly, treatment is aimed at reducing risk and improving prognosis by slowing the progression of the underlying coronary artery disease. Secondly, treatment is aimed at reducing symptoms and improving the quality of life.
The treatment of chronic stable angina is very different from that of unstable angina. As a part of the acute coronary syndrome, unstable angina is treated as an emergency. The treatment of this condition is not covered by this article.
The Importance of Lifestyle
Lifestyle modification plays a key role for the treatment of patients with coronary artery disease including those with angina.
In one study, smoking cessation improved the prognosis for variant angina even during a relatively short follow-up period (20). Smoking after myocardial infarction is associated with more angina and worse health-related quality of life, whereas smokers who quit after their heart attack have similar angina levels and mental health as never smokers (21).

Important risk factors such as diabetes mellitus, hypertension, obesity and lipid abnormalities can all be improved by lifestyle changes. In a large randomized trial called PREDIMED, a Mediterranean diet supplemented with extra-virgin oil or nuts reduced the incidence of major cardiovascular events in patients at high risk of heart disease compared with a control diet aimed at reducing dietary fat (22).
Stress management and exercise training result in improvement of symptoms, in patients with angina (23). Large meta-analyses of exercise-based, cardiac rehabilitation studies have suggested that exercise training reduces cardiac mortality in patients with coronary artery disease (24).
High blood levels of LDL-cholesterol (25) and high triglycerides (26,27) as well as low levels of HDL-cholesterol (28) are all associated with increased risk of coronary artery disease. All these lipid disorders can be improved by lifestyle changes.
Medical Treatment
Daily treatment with low-dose aspirin (75 mg daily) is beneficial and reduces the risk of myocardial infarction and sudden death according to the results of randomized placebo-controlled trials (29). Hence, all patients with angina should receive aspirin therapy unless side effects occur or aspirin intolerance is present (30). Clopidogrel can be offered as an alternative to aspirin when aspirin is not tolerated or contraindicated.
The effectiveness of statin drugs in reducing the risk of cardiovascular events in patients with established coronary artery disease has been well proven (31). These drugs are considered as efficient and safe safe for preventing and treating coronary artery diseases regardless of cholesterol levels. Statins are believed to exert their benefit through lowering of LDL-cholesterol and by reducing inflammatory responses associated with atherosclerosis.
Nitroglycerin was the first drug shown to be effective for angina. In 1879, the English physician, William Murrell, wrote a classic paper in the Lancet called “Nitro-glycerine as a remedy for Angina Pectoris” where he described the physiologic effects of nitroglycerine and recommended its use for the treatment of angina (32).
Nitroglycerin works by dilating both veins and arteries. It may improve blood flow to the myocardium and reduce oxygen demand by dilating the large veins returning blood to the right side of the heart.
Sublingual (under the tongue) nitroglycerin has for long been the mainstay of treatment for angina pectoris. It can be used for acute relief of angina and prophylactically before activities that may precipitate angina. Nitroglycerine spray directed under the tongue has similar effects. Long- acting nitrates taken daily may also reduce the number of angina episodes. Nitroglycerin paste is smeared onto the skin and works in a similar manner. Skin patches are also available.
Beta-blockers are commonly used for the relief of angina and prevention of ischemic events. They work by decreasing the heart rate and myocardial contractility, thereby reducing myocardial oxygen demand.
Calcium channel blockers that slow heart rate (verapamil, diltiazem) can be used to reduce angina in patients who cannot use beta-blockers or in those who do not improve on beta-blockers, nitrates, or both.
Percutaneous Coronary Intervention (PCI)
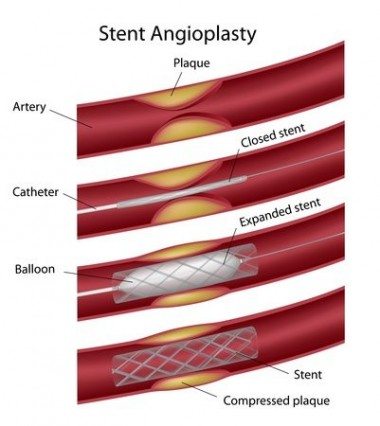
Percutaneous coronary intervention (PCI), commonly known as coronary angioplasty or simply angioplasty, is a non-surgical procedure used to dilate and improve blood flow in blocked coronary arteries. Percutaneous means “through the skin.” The procedure is done by inserting a thin flexible tube into an artery through the skin in the forearm or groin. Usually, a coronary stent, a tube-shaped device, is inserted into the coronary artery.
Patients with a blockage in one vessel treated with PCI show improved exercise tolerance and fewer episodes of angina compared with those who receive medical treatment. However, according to the frequently cited COURAGE-Trial, no difference in the frequency of heart attacks or risk of death has been shown between these two groups (33).
Having said that, it is important to acknowledge that there is overwhelming evidence for the benefits of PCI in patients with acute coronary syndrome (34,35). In these patients, PCI significantly lowers the risk of cardiovascular events and improves survival compared with medical treatment.
Coronary Artery Bypass Grafting (CABG)
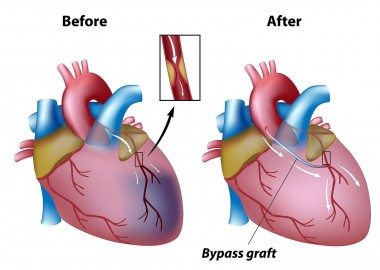
Coronary artery bypass grafting (CABG) is a surgical procedure in which blood is diverted around blocked parts of the coronary arteries to improve blood flow and oxygen supply to the heart muscle. It involves taking a blood vessel from another part of the body, usually the chest, leg or arm, and suturing it to the aorta above and the coronary below the blockage. In this way, blood flow is bypassed around the clogged artery. The new blood vessel is known as a graft.
CABG has been shown to improve quality of life and reduce angina. Patients with significant left main coronary artery disease, widespread coronary narrowing in two or three vessels, diabetes mellitus, or blockages that are unsuitable for PCI are those who do best with CABG.
The Bottom Line
Angina pectoris is commonly experienced among patients with coronary artery disease. In most cases, it s caused by limited blood flow to the heart muscle due to a narrowing or blockage of blood flow in a coronary artery.
Although the patient’s history can sometimes reveal typical angina, diagnostic tests are usually necessary to reveal the underlying cause of the symptoms.
Lifestyle measures are imperative and can improve prognosis and quality of life in patients with angina pectoris and coronary artery disease.
Medical treatment can help relieve symptoms and low-dose aspirin, and statin treatment may improve prognosis.
Invasive measures such as percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) may improve quality of life and improve survival.
Yeah! Axel
But how are your elections
going. Is you is or is you ain’t a ‘Pirate’?.
This is all old news with
‘Heart Business’.
I appreciate your efforts
Axel. But methinks it’s time to look at serious radical/cutting edge
approaches and ‘add ons’ that are beneficial.
People basically don’t
change their diet/lifestyle and nothing will change that. And those
that do are miserable. It’s not even a question of ‘Morality
/Ethics’.
Medicine is not there to
judge anything…but to help fix when people become sick.
People have suffered poor
health through many avenues….Governments, business, misinformation
and so on (a long list).
It’s without doubt that
drugs prolong lives.
Lets forget all the above
and look at other ways that people can improve their quality of life.
Being a MD, people must
frustrate the ‘bejeezus’ out of you.
Here is a list of things:
THAT MAY CHEAT DEATH.
Supplements
Oxygen Therapy (IV
H2O2)
ECPT
Serious ‘Stress
Reduction’
Thinks Michael
Education is what drives most of my writing. People ask questions and maybe some of them will find answers here. Appreciate your comments but not sure I know what you’re getting at this time. About the pirates, well, that’s another story 🙂
Yo! Axel
My apologies for
misunderstanding the concept of your blog.
I failed to realise that
we are not all part of the ‘choir’…and some need to start with the
basics.
My point was: That there
are many unconventional methods that may be of usefulness for people
suffering serious ‘Heart disease’. I mentioned the few that I would
like to see further investigation. And to share experiences with
others who may have found something that they feel has been helpful.
In health
michael
Reference 17 for the Cardiac Magnetic Resonance (CMR) mentions that Cardiac MRI is also known as Magnetic Resonance Imaging (MRI), Nuclear Magnetic Resonance. Why is this called nuclear when, I believe, no radioactive tracer is used except for the MRI contrast agent Gadolinium which is not radioactive?