Estimated reading time: 16 minutes
Coughing is a reflex action where the air is rapidly expelled from the lungs to clear excessive secretions, fluids, or foreign material from the airway. Therefore, cough is an important respiratory defense mechanism. However, coughing may also be a symptom of an underlying disease.
Apart from the discomfort of coughing itself, excessive coughing can cause multisystem problems. For example, it may lead to anxiety, fatigue, insomnia, muscle pain (myalgia), hoarseness (dysphonia), perspiring, and urinary incontinence (1).
Other difficulties, including heightened self-consciousness and changes in lifestyle, are also common consequences of chronic cough (2).
Cough is a common medical complaint. It is estimated to be responsible for approximately 30 million clinicians visits annually in the United States (3)
Most coughs clear up by themselves within three weeks. Such coughs are usually caused by an acute respiratory infection.
Cough is often classified based upon its duration. An acute cough exists for less than three weeks. Cough that has been present for more than three weeks is either subacute (3-8 weeks) or chronic (more than eight weeks) (4).
Several definitions are used when describing cough (5):
- Acute cough: Sudden onset and lasts up to 3 weeks
- Subacute cough: Lasts between 3-8 weeks
- Chronic cough: Lasts for more than 8 weeks
- Productive cough: Cough that brings up phlegm or mucus.
- Dry cough: Cough that does not bring up phlegm or mucus
- Nocturnal cough: Cough that only happens at night
- Hemoptysis: Coughing blood
Acute Cough
Acute cough exists for less than three weeks.
Because acute cough has a different range of causes in adults than it does in children, adults should be assessed and treated differently. The American College of Chest Physicians’ recommends that patients with acute cough be divided into children (younger than 15 years of age) and adults (15 years of age or older) (6).
The overwhelming majority of acute coughs are infectious in origin. These are commonly divided into upper and lower respiratory tract infections.
1. Common Cold
The common cold is the most frequent cause of acute cough. It is caused by a viral infection of the nose and throat and thus classified as an upper respiratory tract infection.
Other symptoms associated with the common cold are a sore throat, runny or stuffy nose, sneezing, low-grade fever, and body aches.
A cold virus enters the body through the upper respiratory tract (mouth, eyes or nose). The virus usually spreads by droplets in the air when someone with common cold coughs, sneezes or talks. It can also spread by hand-to-hand contact with someone who has a cold or through contaminated objects such as toys or telephones.
Children younger than six years are at highest risk of colds. Healthy adults can be expected to have two or three colds annually (7).
Most people recover from a common cold in 7-10 days. However, symptoms often last longer in smokers.
2. Influenza (“the flu”)
Influenza, commonly called the flu, is a viral infection involving the respiratory system. The nose, throat, and lungs are often affected.
Fever, sore throat, headache, nasal congestion, aching muscles, a persistent dry cough, and fatigue are common influenza symptoms
Initially, the flu may seem like a common cold with sneezing, a runny nose, and sore throat. Whereas colds usually develop slowly, influenza tends to come on suddenly. Although a cold can be a nuisance, people typically feel much worse with the flu (8)
Influenza is highly contagious. The viruses travel in droplets spread by coughing and sneezing. These may be inhaled directly or spread by contaminated objects such as towels or telephones.
Usually, influenza resolves on its own. However, the complications of influenza may sometimes become severe and even deadly. This is most likely to occur in young children, old adults, pregnant women, patients with chronic illnesses, and people with a weakened immune system.
Pneumonia is the most severe complication.
The best defense against influenza is annual vaccination.
3. Acute Bronchitis
Acute bronchitis, also known as a chest cold, is a lower respiratory tract infection caused by an inflammation of the bronchial tree.
The bronchial tree consists of tubes (bronchi) that carry air into the lungs. When these tubes get infected, they swell, and mucus (thick fluid) forms inside them (9).

Acute bronchitis lasts for at least five days. It is typically self-limited, resolving within one to three weeks (10).
Cough is the most common symptom of acute bronchitis. It may be with or without sputum production.
Other symptoms include a sore throat, wheezing, shortness of breath, fever, chest discomfort, chills, and body aches.
Acute bronchitis is most often caused by a viral infection. These may even be the same viruses that cause the common cold.
Acute bronchitis may sometimes be caused by bacterial and fungal infections (9).
Exposure to irritants, such as smoke, dust, or fumes, also can cause acute bronchitis.
Acute bronchitis is usually a presumptive diagnosis, based on history and examination, when the patient presents with an acute, and typically productive, cough of less than three weeks’ duration.
Fever is not common in people with acute bronchitis. However, having a fever can be a sign of another condition, such as the flu or pneumonia (10).
Treatment is focused on patient education and supportive care. Antibiotics are not needed for the vast majority of patients. Antibiotics are greatly overused for this condition (8).
One of the reasons antibiotics are described is that many doctors are worried that they might miss a case of acute community-acquired pneumonia, which still has a relatively high mortality, especially among the elderly (11).
4. Pneumonia
Pneumonia is an inflammation caused by an infection of the air sacs in the lungs.
The infection may be caused by bacteria, viruses, and fungi.
Community-acquired pneumonia is the most common type of pneumonia. It occurs outside of hospitals.
Pneumonia may be a complication of another condition, such as influenza.
Pneumonia is more likely to occur in patients with underlying chronic diseases such as chronic obstructive pulmonary disease (COPD), asthma or heart failure.
Patients with pneumonia often have a fever and a productive cough. Other symptoms include chills, chest pain, and difficulty breathing.
Hospital-acquired pneumonia occurs during a hospital stay, usually when patients are being treated for another illness. It may be serious because these patients are often more vulnerable and the bacteria responsible may be resistant to antibiotics.
5. Whooping Cough (Pertussis)
Whooping cough is a highly contagious respiratory infection affecting the airways and lungs.
It is caused by a type of bacteria called Bordetella pertussis which spreads in the droplets of the coughs or sneezes of someone with the infection (12).
The first symptoms are usually similar to those of a common cold, such as a sore throat and a runny nose. About a week later, a severe hacking cough often develops, sometimes followed by a high-pitched intake of breath that sounds like “whoop.”
However, many patients don’t develop the classic whoop.
The coughing bouts usually last a few minutes at a time. The coughing usually brings up thick mucus, sometimes followed by vomiting.
Today, whooping cough primarily affects children too young to have completed the full course of vaccinations and teenagers and adults whose immunity has faded (13). Vaccination secures immunity for no more than a few years.
Adult patients often have an atypical mild disease course with a nonspecific dry cough.
6. Worsening of Chronic Obstructive Pulmonary Disease (COPD)
While chronic obstructive pulmonary disease (COPD) is mainly a chronic disease, a substantial number of patients suffer from exacerbations characterized by worsening or “flare up” of symptoms.
In many cases, the worsening is from an infection of the airways or lungs or from inhaling irritating substances from the environment. However, in many cases, the cause is unknown.
Typical symptoms include more breathlessness than usual, a change in sputum (color or amount), increased cough, more tiredness (fatigue), trouble sleeping and in some cases, a fever (14).
7. Pulmonary Embolism (PE)
Pulmonary embolism is a blockage in one or both of the pulmonary arteries within the lungs.
It is caused by blood clots that travel from the lower extremities, through the right heart chambers, and lodge in the lungs. Pulmonary embolism can be life-threatening (15).
In most cases, a blood clot in the deep veins of the leg, called deep vein thrombosis (DVT), is the underlying cause of pulmonary embolism. Painful swelling of one leg, ankle or feet should raise the suspicion of DVT (16).
The most common symptoms of pulmonary embolism include shortness of breath, cough, and sometimes chest pain that gets worse when breathing (pleuritic pain). Signs of DVT in one or both legs may be found.
8. Acute Inhalation Injury
Inhaled substances may cause injury to the airways and lead to acute cough. This may occur at various places including the home and workplace (17).
Examples of common chemical irritants are ammonia, hydrogen chloride, hydrogen sulfide, hydrogen fluoride, sulfur dioxide, oxides of nitrogen, and chlorine.
Smoke inhalation from fires is common among firefighters and non-occupational victims.
Individuals who are accidentally exposed to toxic gases usually recover completely. However, sometimes acute life-threatening or chronic severe complications may develop (18).
Subacute and Chronic Cough
A cough that has been present for more than three weeks is either subacute (3-8 weeks) or chronic (more than 8 weeks) (4).
9. Postinfectious Cough
Patients may complain of a persistent cough following acute respiratory infections such as the common cold or acute bronchitis.
If a cough lasts for more than three weeks, it is no longer considered to be an acute cough. Instead, it falls into the category of a subacute cough.
One study found that postinfectious cough was the most common cause of subacute cough. The study also found that such cough frequently resolves without specific therapy (19).
10. Upper Airway Cough Syndrome (UACS)
The American College of Chest Physicians defines upper airway cough syndrome (UACS) as a syndrome characterized by chronic cough (i.e., present for ≥8 weeks) related to upper airway abnormalities (20).
UACS is typically associated with postnasal drip and the presence of mucus in the throat (21).
Postnasal drip occurs when excessive mucus is produced by the mucosal cells that line the nasal cavity. The excess mucus accumulates in the throat or at the back of the nose (nasopharynx) (22).
Symptoms of postnasal drip include frequent nasal discharge and a sensation of liquid dripping in the back of the throat (4). This is often followed by frequent throat clearing. However, many patients with postnasal drip don’t experience these symptoms. In these cases, chronic cough may be the sole complaint.
Several remedies for UACS may be helpful. A humidifier or steam inhalation may be useful. Keeping well hydrated may help keep the mucus thinner. In some cases, sleeping on propped up pillows may prevent the mucus from collecting at the back of the throat (23).
Nasal irrigation, usually available over the counter, may help and so can oral decongestants such as pseudoephedrine (as in Sudafed) or phenylephrine (as in Sudafed PE or Neo-Synephrine). Guaifenesin (as in Mucinex) is a medication that can thin the mucus (23).
Antihistamines (diphenhydramine, chlorpheniramine, loratadine, desloratadine, fexofenadine, cetirizine levocetirizine) and nasal decongestants may be helpful. However, nasal decongestants should only be used for a day or two as more extended treatment may make the situation worse.
11. Asthma
Asthma is the second leading cause of chronic cough in adults, and the most common cause in children (24).
Asthma is a condition in which the airways narrow and swell and produce extra mucus. This can cause shortness of breath, wheezing, tightness in the chest, and a nonproductive cough (25).
Some patients with asthma have infrequent attacks or have symptoms under certain conditions, such as when exercising, while others have more frequent or chronic symptoms.
Allergy-induced asthma is triggered by airborne substances such as pollen, spores, dust mites, and pet dander. Other allergic symptoms such as watery eyes and runny nose are common.
Exercise-induced asthma is typically provoked by exercise and often gets worse when the air is cold and dry.
Occupational asthma is usually triggered by workplace irritants such as chemical fumes or dust.
12. Gastroesophageal Reflux
Gastroesophageal reflux is believed to be the second or third most common cause of chronic cough (4).
Gastroesophageal reflux disease (GERD) is a chronic digestive disease that occurs when stomach acid or, occasionally, stomach content, flows back (reflux) into the esophagus. The reflux irritates and may damage the lining of the esophagus causing the disease (26).
Most healthy people experience acid reflux and heartburn once in a while. However, when these symptoms occur at least twice each week or interfere with daily life, GERD should be suspected.
However, many patients with GERD don’t experience acid reflux or heartburn. In these cases, cough may be the only symptom.
Most people can manage the symptoms of GERD with lifestyle changes and over-the-counter medications. But some patients may need prescription drugs, or even surgery, to reduce symptoms.
Proton pump inhibitors such as Nexium, Protonix, Prevacid, Aciphex, or Prilosec are particularly helpful.
13. Laryngopharyngeal Reflux (LPR)
Laryngopharyngeal reflux (LPR) is a condition that develops when stomach acid travels up into the throat. Although some patients also experience “heartburn” or “indigestion,” many do not have these complaints.
Typical symptoms include chronic cough, hoarseness (dysphonia), frequent throat clearing, sore throat and difficulty swallowing (27).
Most of the time, LPR is well controlled with lifestyle changes and medications (proton pump inhibitors).
14. Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) is a relatively common sleep disorder with several potentially serious consequences. It causes breathing to stop and then start again intermittently during sleep (28).
OSA occurs when the throat muscles intermittently relax and block the airways during sleep causing a repetitive obstruction of the upper airway during sleep.
OSA may seriously affect the quality of life and is strongly associated with the risk of diabetes, high blood pressure, liver disorders, and cardiovascular disease.
Recent reports have shown a resolution of chronic cough in many patients following treatment of concomitantly diagnosed OSA (29).
However many patients with OSA also suffer from gastroesophageal reflux disease (GERD), upper airway cough syndrome (UACS), and cough related asthma. Whether cough in patients with OSA is caused by these disorders or directly related to the OSA itself is unknown.
15. Chronic Bronchitis
Chronic obstructive pulmonary disease, or COPD, refers to a group of conditions that cause airflow blockage leading to shortness of breath, cough, mucus (sputum) production and wheezing. It includes emphysema, chronic bronchitis, and in some cases asthma (25).
Tobacco smoke is the leading cause of the development and progression of COPD (30).
COPD was the third leading cause of death in the United States in 2014 (31).
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD.
Chronic bronchitis is defined as a productive cough that lasts at least three months, with recurring bouts occurring for at least two consecutive years. It is caused by an inflammation of the lining of the bronchial tubes leading to shortness of breath, a daily cough and mucus production. Almost all patients are smokers.
16. Bronchiectasis
Bronchiectasis is a condition in which damage to the airways (bronchi) causes them to widen and become flabby and scarred (32). It usually results from repeated or persistent inflammation of the airways.
In bronchiectasis, the airways slowly lose their ability to clear out mucus. Consequently, mucus builds up and creates an environment in which bacteria can grow, leading to repeated, serious lung infections.
Cough is a major symptom of bronchiectasis.
17. Interstitial Lung Disease (ILD)
The term interstitial lung disease (ILD) refers to a broad category of lung diseases rather than a distinct disease entity. Hence, it includes a variety of illnesses with different underlying causes. These disorders are grouped together because of similarities in their clinical presentations, radiographic appearance, and physiologic features (33).
The abnormalities that characterize ILD involve the lung interstitium (the area between the capillaries and the alveolar space) to a greater extent than the alveolar spaces or airways. The interstitium supports the delicate relationship between the alveoli and capillaries, allowing an efficient gas exchange (25)
The lungs may be initially injured by external exposure (e.g., asbestos, drugs, moldy hay), an underlying autoimmune disease (e.g., rheumatoid arthritis) or some unknown agent (idiopathic pulmonary fibrosis).
Lung function may become severely reduced in ILD. Gas exchange is impaired, and the work of breathing is increased because of decreased lung compliance.
Shortness of breath and a nonproductive cough are the most common symptoms.
Therapy depends on the underlying disease and may consist of immunosuppressive drugs and avoidance of disease-inducing exposures.

18. Lung Cancer
Evidence suggests that less than 2 percent of chronic cough is caused by lung cancer (34).
Other symptoms associated with lung cancer include chest pain, breathlessness and coughing up blood (hemoptysis)(25).
Smoking is the most significant risk factor for lung cancer.
19. Heart Failure
Patients with heart failure may experience a persistent cough or wheeze with white or pink blood-tinged phlegm (35).
Heart failure occurs when the heart muscle is weakened and cannot pump enough blood to meet the body’s needs for blood and oxygen. In some cases, the pumping capacity of the heart muscle is preserved, but the left ventricle is stiff with decreased compliance and impaired relaxation, leading to increased filling pressure in the left ventricular chamber (25).
Heart failure is caused by an underlying heart disease that has caused damage to the heart muscle and/or increased stiffness of the heart muscle. Coronary heart disease, hypertension, valvular disorders, and dilated cardiomyopathy are the most common causes of heart failure.
Heart failure frequently presents with shortness of breath on exertion, fatigue, diminished exercise tolerance, and fluid retention.
20. Ventricular Premature Beats
Ventricular ectopic or premature beats are due to electrical activity originating from the ventricles of the heart.
Many patients with ventricular premature beats experience palpitations. Palpitations are defined as an unpleasant awareness of heart muscle contractions in the chest (36).
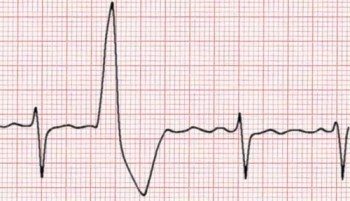
Evidence suggests that ventricular premature beats may cause chronic cough (37).
Subjects with cough induced by premature ventricular beats may have a more severe perception of arrhythmia symptoms than subjects without cough (38)
21. Angiotensin Converting Enzyme (ACE) Inhibitors
Angiotensin converting enzyme (ACE) inhibitors are commonly used to treat hypertension.
These drugs affect the renin-angiotensin-aldosterone system and block the conversion of angiotensin I to angiotensin II, which is involved in vasoconstriction.
A nonproductive cough is a well-recognized side effect of treatment with ACE inhibitors occurring in up to 15 percent of patients treated with these agents (39).
This type of cough typically resolves within 1-4 days following discontinuation of the drug, but can take up to 4 weeks (4).
22. Smoker’s Cough
A smoker’s cough is a chronic cough that often develops among smokers.
Initially, it may be a dry cough, but over time it usually becomes productive.
A smoker’s cough is usually worse upon awakening in the morning.
A chronic cough among long-term smokers is often due to an underlying disease such as chronic bronchitis or lung cancer.
The best treatment for smoker’s cough is to quit smoking altogether. While cough may sometimes worsen initially after stopping, it almost always improves with time.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.



What about cough during chemotherapy ?
Good point Jeff.
Maybe Chemo Cough should be listed as well.
Thanks.
Can a cough associated with allergies/asthma come from changes in the weather? If so, can you tell me why/how does this happen. Thanks for your articles.
Have a girl friend has had a cough for about 3 years and has had different test and not able to cure her, she is desperate now.
Margo Izabal