Estimated reading time: 12 minutes
Chest pain is a common symptom associated with a variety of underlying causes.
More than six million people visit hospital emergency departments in the United States each year because of chest pain (1).

The cause of chest pain may vary from life-threatening conditions to those that are relatively harmless.
Chest pain is most commonly caused by disorders of muscles, ligaments, tendons, and bones. Such pain is often called musculoskeletal pain and is usually harmless.
Digestive disorders are also a common cause of chest ache.
It is practical to classify the underlying conditions causing chest pain into;
- cardiac (heart conditions)
- pulmonary (lung conditions)
- gastrointestinal (caused by digestive disorders)
- musculoskeletal (disorders of muscles, ligaments, tendons, and bones)
- psychiatric
- other
Nowadays, all chest pain is regarded as suspected heart disease until proven otherwise.
Actually, most emergency departments have chest pain units, a fast-track service for patients with chest pain.
History Is a Key Factor
History and physical examination are of crucial importance when determining the cause of chest pain.
The character or quality of pain is essential. Sometimes, there may be only a vague discomfort. In other cases, the pain may be sharp, ripping or tearing, or just a feeling of pressure, fullness, or tightness in the chest.
The localization of the pain may also help determine its origin.
Pain in the middle of the chest may be caused by heart disease or digestive disorders. In contrast, right or left sided chest pain often originates from the ribs or muscles and tendons in the chest cage.
Chest pain may also radiate to other parts of the body. For example, pain due to coronary artery disease may radiate to the neck, jaw, and arms.
In addition, knowing the onset of pain is helpful. An abrupt onset may suggest pneumothorax and aortic dissection.
Chest ache that lasts only for a few seconds is unlikely to be caused by coronary artery disease. The same is true for pain that is consistent over weeks to months (2).
Furthermore, if and how the pain may be provoked is of importance.
For example, so-called pleuritic chest pain typically worsens with respiration. Such pain is often left or right sided.
Chest pain provoked by exertion is typical of angina pectoris (3).
Pain made worse by swallowing is likely of esophageal origin.
Chest ache associated with body position or specific movements is likely to originate from muscles and tendons. In addition, such pain is often well-localized and associated with tenderness on palpation (pushing on the spot).
Cardiac Causes – Heart Conditions Causing Chest Pain
1. Heart Attack/Acute Coronary Syndrome (ACS)/
Acute heart attack and acute coronary syndrome (ACS) are different terms used to describe the same phenomenon.
ACS covers a range of conditions associated with a sudden obstruction of blood flow in a coronary artery. Patients with ACS typically experience pressure, fullness, or tightness in the chest. Sometimes there is searing pain that may radiate to the back, neck, jaw, shoulders, and arms, particularly the left arm.
The pain usually lasts more than a few minutes.
If there is a complete blockage of a coronary artery, the pain may last for several hours. Moreover, it may be associated with shortness of breath, cold sweats, dizziness or weakness, nausea, and vomiting.
ACS should always be treated as an emergency.

2. Angina Pectoris
Angina pectoris is often described as a pressure or a squeezing sensation in the chest. The discomfort may radiate to the shoulders, arms, neck, jaw, or the back region between the shoulder blades.
Angina pectoris is not a disease. It is a symptom usually caused by inadequate blood flow in a coronary artery. Hence, in most cases, angina reflects underlying coronary artery disease (3).
Typically, a patient with angina will experience no symptoms at rest. However, during exercise, the oxygen demands of the heart muscle will increase. If blood supply in a coronary artery is limited, usually because of blockage in a coronary artery, angina will occur. If the patient stops exercising, the oxygen supply will again meet demands, and angina will resolve.
3. Aortic Dissection
Aortic dissection occurs when there is a tear in the inner layer of the aorta (the large blood vessel branching off the heart).
The tear causes the inner and middle layers of the wall of the aorta to become separated. This may cause the outer wall of the aorta to rupture, causing fatal bleeding.

Patients with acute aortic dissection usually present suddenly with severe, sharp pain in the chest. The pain sometimes radiates to the back (4).
Aortic dissection is relatively rare. It is a medical emergency and always needs immediate treatment.
4. Pericarditis
Pericarditis is an inflammation (swelling) of the pericardium. The pericardium is a thin membrane or sac surrounding the heart.
In most cases, a viral infection is responsible.
The primary symptom may be a sudden, sharp, and stabbing pain behind the sternum (breastbone). However, sometimes there may only be a dull ache.
The pain of pericarditis typically worsens when lying down or breathing in (pleuritic pain). Moreover, it may often get better when sitting up and leaning forward.
Pericarditis is usually not a serious condition and hospital admission is seldom required.
Symptoms usually resolve within a week. However, some patients experience recurring symptoms lasting longer than three months.
5. Stress Cardiomyopathy (Takotsubo)
Stress cardiomyopathy, also called the broken heart syndrome, apical ballooning syndrome, or takotsubo cardiomyopathy was first described in 1990 in Japan.
The symptoms of stress cardiomyopathy mimic those of an acute heart attack. However, it is an entirely different disorder and is not caused by blocked coronary arteries.
Patients with stress cardiomyopathy experience sudden, intense chest pain.
An emotionally stressful event usually precipitates the pain, hence the term “broken heart syndrome.”
The stressful event could, for example, be the death of a loved one, breakup of a relationship, domestic abuse, devastating financial losses, or a natural disaster (5).
Stress cardiomyopathy is also characterized by a severely decreased contraction of a part of the heart muscle.
However, although the heart muscle’s function may be severely affected during the initial phase, recovery is usually complete.
Pulmonary Causes – Lung Conditions Causing Chest Pain
6. Pulmonary Embolism
Pulmonary embolism is a blockage in one or both of the arteries within the lungs. It is caused by blood clots that travel from the lower extremities, through the right heart chambers, and lodge in the lungs. Pulmonary embolism can be life-threatening (6).
In most cases, a blood clot in the leg’s deep veins, called deep vein thrombosis (DVT), is the underlying cause.
Sitting for extended periods, such as during long flights, may increase DVT risk (7).
Shortness of breath is the most common symptom. Cough is also relatively common and some patients have chest pain that gets worse when breathing (pleuritic pain).
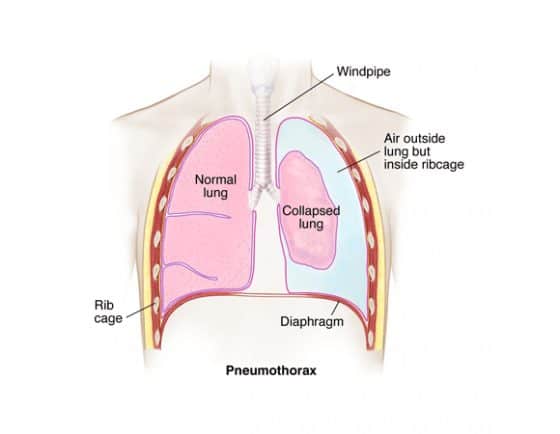
7. Pneumothorax
A pneumothorax is when air builds up between the outside of the lung and the inside the chest wall (8). The air can come from the lung or from outside the body if there is a chest injury. A large pneumothorax may compress the lung, causing it to collapse.
Pneumothorax caused by leaks of air from the lungs usually occurs in people with a lung condition. However, it can also occur in people who are otherwise entirely healthy (spontaneous pneumothorax).
Spontaneous pneumothorax is far more common in men than in women. It often occurs in people between 20 and 40 years old and is most common in tall individuals.
The pneumothorax pain is usually sudden in onset and gets worse by breathing in (pleuritic pain).
The treatment of pneumothorax depends on its size and whether it’s expanding. A small pneumothorax may not need any treatment as it will heal on its own. However, a large pneumothorax will need to be drained using a syringe or a chest tube.
8. Pneumonia, Asthma, and Chronic Obstructive Lung Disease (COPD)
Pneumonia may cause chest pain. The pain often gets worse on inspiration (pleuritic pain). However, many patients with pneumonia don’t have chest pain.
Patients with pneumonia often have a fever and a productive cough as well.
Patients with asthma and chronic obstructive lung disease (COPD) typically suffer from shortness of breath. However, during worsening of these disorders, patients often describe chest tightness that may sometimes be interpreted as chest pain.
9. Pleuritis (Pleurisy)
Pleuritis or pleurisy is an inflammation (swelling) of the membranes (pleurae) covering the lungs (9)
The chief symptom associated with pleurisy is a sharp, stabbing pain in the chest. Patients often experience chest pain when breathing (pleuritic pain).
The most common underlying cause is a viral infection.
Treatment of pleuritis depends on the underlying cause. Paracetamol and NSAID’s such as ibuprofen may help relieve the pain.
10. Lung Cancer
Patients with lung cancer often complain of chest pain. The pain is usually located on the same side as the tumor.
Other symptoms include cough, hemoptysis (coughing blood), and shortness of breath.
Also, chest ache associated with lung cancer often gets worse with deep breathing, coughing, or laughing (10).
11. Pulmonary Hypertension
Pulmonary hypertension is a condition caused by elevated pressure (hypertension) in the pulmonary arteries (11).
Although shortness of breath is the main symptom of pulmonary hypertension, some patients may experience chest pain. The pain is usually most pronounced during exertion.
Gastrointestinal Causes – Digestive Disorders Causing Chest Pain
12. Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD) is a common cause of chest discomfort (12).
GERD is a chronic digestive disease that occurs when stomach acid or, occasionally, stomach content flows back (reflux) into the esophagus. The reflux irritates and may damage the lining of the esophagus, causing the disease.
Most healthy people experience acid reflux and heartburn once in a while. However, when these symptoms occur at least twice each week or interfere with daily life, GERD should be suspected.
The chest pain associated with GERD is often described as squeezing or burning. It is usually located behind the sternum (substernal pain). Sometimes it radiates to the back, neck, jaw, or arms. It is usually relieved by antacids.
Most people can manage the symptoms of GERD with lifestyle changes and over-the-counter medications. Nevertheless, some patients may need prescription drugs, or even surgery, to reduce symptoms.
13. Esophagitis
The term esophagitis describes an inflammation or swelling of the esophagus.
Heartburn is the most common symptom of esophagitis. Other common symptoms include upper abdominal discomfort, nausea, bloating, and fullness.
Musculoskeletal Causes of Chest Pain
The term musculoskeletal is used to describe pain associated with muscles, ligaments, bones, and tendons.
14. Musculoskeletal Chest Pain
A large proportion of chest pain is caused by underlying conditions of muscles, ligaments, bones, and tendons.
This type of pain is usually referred to as musculoskeletal pain.
The chest wall contains a range of bony and soft tissue structures, including the spine. Hence, it may be difficult to pinpoint the exact source of pain in an individual patient.
Musculoskeletal conditions may cause both left and right-sided chest pain. Sometimes the pain gets worse when breathing.
The ache is often associated with body position or specific movements. Furthermore, it is usually well localized and associated with tenderness when pushing on the spot.
Psychiatric Causes of Chest Pain
15. Anxiety Chest Pain and Panic Disorder
Chest pain may be a symptom of anxiety (13).
Anxiety chest pain is often described as a sharp, stabbing sensation. The pain often starts suddenly and is usually not related to physical exertion.
Sometimes, however, there may be a less sharp, dull ache in the chest that is more persistent.
Panic disorder is an anxiety disorder characterized by recurrent unexpected panic attacks (14).
Panic attacks are sudden episodes of extreme fear or distress, often associated with chest pain and fast heartbeat. The patient may also experience palpitations (15), sweating, shortness of breath (16), and numbness.
Patients with panic attacks often suffer from constant fear about having further attacks. Thus, they ususllay try to avoid places or circumstances where attacks have occurred before.
It has been suggested that approximately one-quarter of patients seeking chest pain treatment have panic disorder (17). Notwithstanding, panic disorders often go unrecognized and untreated, leading to frequent return visits to emergency departments.
Fortunately, panic disorder is treatable, and quality of life can be improved by psychological methods and drug therapy (18,19).
Other Causes of Chest Pain
16. Chest Pain Related to Drug Abuse
Several illegal drugs can have adverse effects on the heart, ranging from abnormal heart rate to heart attacks.
Cocaine is an illegal drug most often associated with visits to hospital emergency departments in the United States.
Cocaine use has been related to both chest pain and heart attacks.

17. Herpes Zoster
Herpes zoster (shingles) is an infection caused by the varicella-zoster virus, the same virus which causes chickenpox.
The chickenpox virus may remain dormant in the nervous system for years. In herpes zoster, it becomes activated again.
Herpes zoster is characterized by a red skin rash that can cause pain and burning. Typically it occurs as a stripe of blisters on one side of the body, often on the torso, neck, or face.
Most cases of herpes zoster clear up within two to three weeks. Approximately 1 in 3 people in the United States will have herpes zoster at some point in their life (22).
Chest pain may be the presenting symptom of herpes zoster. The diagnosis may be tricky because the pain usually precedes the rash.
The article was initially published in 2017.
It was revised, updated and republished on January 17th, 2021.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

Thank you! This is quite helpful.