Estimated reading time: 12 minutes
Swollen feet and swollen ankles are common reasons why people seek medical advice. I’m not talking about inflammation due to injury or infection, but a medical condition commonly called leg edema.
Leg edema is not only undesirable due to cosmetic reasons but may lead to thinning of the skin, discoloration or staining (pigmentation) and skin sores (ulcers). Healing may be slow, and there is increased risk of infection.

Edema is defined as a palpable swelling caused by an increased volume of fluid in a tissue. The fluid accumulation is usually located in the interstitium, the tissue or space between the cells (extracellular space).
Edema can be generalized and localized. Generalized edema is a state were increased fluid volume is found in most organs of the body whereas localized edema is only found in certain body parts. Leg edema with swollen ankles and feet is the most common type of localized edema.
The most common cause of leg edema in people over age 50 is chronic venous insufficiency, a condition that affects up to 30 percent of the population. In women under 50 years old, the most likely cause of edema is idiopathic edema, formerly known as cyclic edema.
In some cases, edema may be a sign of a more serious underlying medical condition such as heart failure, liver cirrhosis or kidney disease. The medical history and physical examination will usually reveal whether these disorders are present or not.
Why Does Edema Occur?
Edema mainly occurs through two underlying mechanisms.
Firstly, fluid from the capillaries may move or leak into the interstitial space. This is usually caused by an alteration in pressure conditions (increased pressure) within the capillaries and increased capillary permeability.
The capillaries are the smallest blood vessels. They are localized between the arteries and the veins and connect these two parts of the circulatory system. They serve to distribute oxygenated blood from arteries to the tissues and to transport blood from the tissues back into the veins.
The second fundamental mechanism in edema formation is the retention of dietary sodium and water by the kidneys
When fluid moves from the capillaries into the interstitium, the volume within the circulation (plasma volume) diminishes and tissue perfusion is reduced. The kidneys, which play an important regulatory role, respond by retaining sodium and water to preserve plasma volume and maintain normal tissue perfusion. However, this response may lead to more fluid entering the interstitium, thereby further promoting edema formation.
Some renal diseases and kidney failure may cause an inappropriate fluid retention by the kidneys. In these cases, the retention of sodium and water occurs despite adequate plasma volume and normal tissue perfusion.
Chronic Venous Insufficiency
Chronic venous insufficiency is the most common cause of leg edema in western nations. An estimated 40-50 percent of the adult population in the United States suffer from the disorder (1).
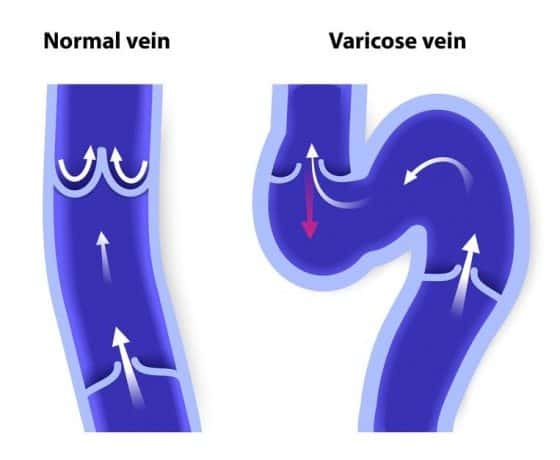
Veins are the blood vessels that return blood from the arms, legs, and organs back to the heart. Venous insufficiency is a condition in which the flow of blood through the veins is impaired.
Normally there is continuous flow of blood from the limbs back toward the heart. Valves within the veins of the legs prevent the backflow of blood. In venous insufficiency, blood flow through the veins is obstructed, or there is backward leakage of blood flow through damaged valves. In many cases, obstruction and backward leakage coexist. Consequently, venous pressure is increased (venous hypertension) increasing the risk of fluid entering the interstitium through the walls of the capillaries.
Many patients with chronic venous insufficiency have a history of deep vein thrombosis (DVT), and varicose veins are common. However, a history of DVT is obtained in less than one-third of patients (2). The term postthrombotic syndrome is often used to describe symptoms from chronic venous insufficiency resulting from previous DVT (3,4).
The leg muscles play a significant role in returning venous blood from the legs as they help to squeeze blood forward. In some cases, inadequate muscle pump function, for example, due to weakness of the leg muscles or immobilization, may contribute to venous insufficiency.

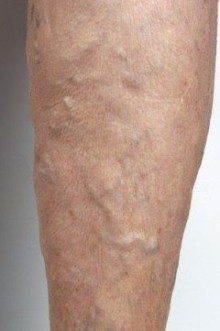
Venous insufficiency in the legs is characterized by swelling of the legs due to edema, discoloration of the skin (pigmentation), and prominent varicose veins (ropy veins). Skin ulcers may develop, and some patients have aching, cramping, and burning sensation in the legs and feet.
Telangiectasias and reticular veins, sometimes called spider veins, are dilated veins within or directly under the skin. These are commonly found in people with chronic venous insufficiency. Women are more commonly affected than men (5).
Varicose veins are dilated, elongated, tortuous, veins under the skin, three millimeters or greater in diameter. Varicose veins are present in 30-40 percent of the general population (6)
Risk Factors for Venous Insufficiency
Several factors increase the risk of venous insufficiency (7). The most common are the following:
- A history of deep vein thrombosis (DVT)
- Varicose veins
- Age over 50
- Female sex
- Family history of varicose veins
- Obesity
- Pregnancy
- Inactivity
- Smoking
- Extended periods of standing or sitting
How Is Venous Insufficiency Diagnosed?
Localized edema of the lower extremities and pigmentation strongly suggests venous insufficiency. The presence of telangiectasias and varicose veins may support the diagnosis. The medical history and physical examination are important to exclude other causes of edema.
Leg edema is usually detected by the presence of pitting. After pressure is applied to the affected area pitting should remain for at least five seconds. Pitting reflects the movement of tissue fluid in response to pressure.
The absence of pitting may suggest other causes of edema such as lymphatic obstruction or hypothyroidism. Pretibial myxedema is a type of non-pitting edema sometimes found in patients with thyroid disease and is associated with localized areas of swelling.
Duplex ultrasound examination is a useful method to confirm the presence of venous obstruction or valvular insufficiency. It is a relatively simple, non-invasive procedure based on ultrasound and Doppler assessment to demonstrate the presence and extent of venous insufficiency. The majority of symptomatic patients should undergo duplex ultrasound to evaluate the extent of venous disease, which impacts the choice of treatment.
General Treatment of Venous Insufficiency
Several general measures are helpful to reduce symptoms and improve well-being in people with chronic venous insufficiency. Among these are:
- Avoid extended periods of standing or sitting
- During long periods of sitting or standing, periodically flexing and extending the legs, feet, and ankle may be helpful.
- Regular exercise, such as walking is helpful
- Weight loss is beneficial among those who are overweight or obese.
- Elevate the legs whenever possible
- Wear compression stockings
- Proper skin hygiene is recommended

Compression stockings can be purchased at most pharmacies and medical supply stores and come in various styles, including below-the-knee, above-the-knee and pantyhose styles. They also come in different compressions varying from 8 to 10 mm Hg, up to 40 to 50 mm Hg. Knee-high stockings are sufficient in most cases.
The stockings apply the greatest amount of pressure at the ankles, and the pressure gradually decreases up the leg. This helps to pump blood back through the veins.
Nonsurgical Treatment
Several nonsurgical therapies are available for chronic venous insufficiency.
Sclerotherapy involves the injection of a special solution directly into spider veins or small varicose veins that causes them to collapse and disappear. Sclerotherapy can reduce pain and discomfort and is often performed for cosmetic reasons as well.
Endovenous thermal ablation uses laser or high-frequency radio waves to create heat to close up the affected vein. There is minimal bleeding and bruising compared with surgical techniques.
Surgical Treatments
Surgical technique options include vein ligation and stripping, microincision/phlebectomy, and bypass surgery.
Vein ligation aims at surgically tying off the affected veins. Stripping is the surgical removal of larger veins through two small incisions and is usually a more extensive procedure than ligation. Ligation and stripping often are performed in together in the same patient.
Microincision/phlebectomy removes the affected veins through a small incision or needle puncture.
Vein bypass involves using a healthy vein transplanted from elsewhere in the body to reroute blood around the affected vein. It is usually reserved for more severe cases affecting the upper part of the leg.
Deep Vein Thrombosis (DVT)
A blood clot in the deep veins of the leg, called deep vein thrombosis (DVT), may cause leg edema. The edema is mostly confined to the feet or ankles and usually only affects one side whereas most other causes of leg edema involve both legs.
DVT may also cause leg pain. Painful swelling of one leg, ankle or feet should raise the suspicion of DVT.
DVT may be a serious condition because blood clots can break loose, travel through the bloodstream and lodge in the lungs, a condition called pulmonary embolism.
There are several risk factors for DVT. Among them are inherited disorders of blood clotting, prolonged bed rest, injury or surgery, pregnancy, birth control pills, smoking, and some forms of cancer.
Sitting for long periods such as during long flights may also increase the risk of DVT because the leg muscles are not contracting. The leg muscles play a major role in pumping the blood through the veins. The most effective preventive measure is to contract the leg muscles, either while sitting or by walking when possible.
DVT is usually treated with blood thinners (antithrombotic drugs).
Lymphedema
Lymphedema refers to swelling of the arms or legs resulting from obstruction of flow in the lymphatic system (8). The system is composed of lymph nodes and a network of lymphatic vessels that carry a clear fluid called lymph. The lymphatic system connects directly with the blood circulation. The lymph vessels empty into the lymphatic ducts, which drain into one of the two subclavian veins.

Surgical removal of lymph nodes can cause swelling of a limb. This is most common following treatment for breast cancer which often includes axillary lymph node dissection. This may cause swelling of the arm. Inguinal lymph node dissection in patients with melanoma can cause lymphedema of one or both legs.
Radiation treatment for cancer may also cause lymphedema.
Lymphedema may be associated with inflammatory conditions such as rheumatoid arthritis.
Worldwide, the most common cause of lymphedema is lymphatic filariasis, an infection with the filarial worms. These parasites are transmitted to humans through the bite of an infected mosquito and develop into adult worms in the lymphatic vessels, causing severe damage and lymphedema. Elephantiasis, a painful swelling of the legs and genital organs, is a classic sign of late-stage filariasis. The infection can usually be treated with drugs.
Drug Induced Edema
Some drugs may cause edema by reducing the excretion of sodium through the kidneys. Sodium retention increases fluid retention.
Drugs that dilate or expand arteries may sometimes cause edema. Such drugs were often used in the past to treat high blood pressure but are seldom used today. Examples are diazoxide, minoxidil, and nifedipine.
Calcium channel blockers of the dihydropyridine group are commonly used to treat high blood pressure (9). Examples are amlodipine, felodipine, isradipine, and lercanidipine. These drugs often cause leg edema due to leakage of fluid from the capillaries to the interstitial space.
Leg edema may occur in 4-6 percent of patients with diabetes treated with thiazolidinedione drugs such as pioglitazone and rosiglitazone.
Nonsteroidal anti-inflammatory drugs (NSAID’s) can increase edema formation in patients with underlying conditions such as heart failure or cirrhosis (10).
Estrogens such as those used in oral contraceptives may sometimes promote sodium retention and cause edema.

Swollen Feet and Swollen Ankles During Air Travel
It is quite common to experience swollen feet and swollen legs during air travel. The combination of inactivity and sitting with the legs down on the floor may cause blood to pool in the veins. The inactivity of the leg muscle adds further to the problem because contracting these muscles help to squeeze blood forward.
To reduce swelling of the feet and legs during a flight, it may be helpful to extend the ankles and knees when seated and take a short walk whenever possible. Avoiding alcohol and sedatives is recommended. Drinking plenty of water may help to prevent dehydration but carbonated drinks should be avoided as they may cause bowel discomfort.
Generalized Edema
Generalized edema affects most organ in the body. The most common causes are heart failure, liver cirrhosis, kidney disease, premenstrual edema, and pregnancy.
Massive and generalized edema cause by excess fluid accumulation is called anasarca.
Intermittent edema is a common premenstrual symptom.
The Take-Home Message
Leg edema is a common reason why people seek medical attention.
Chronic venous insufficiency is the most common cause of leg edema in western nations.
Other causes of leg edema such as heart failure, renal disease, and thyroid disease should be excluded.
Some drugs may cause edema.
Leg edema is common during air travel.
Acute swelling of one leg may suggest deep vein thrombosis (DVT).
The treatment of edema depends on the underlying cause. Reducing the amount of sodium in the diet may be helpful and so can general measures such as avoiding long periods of standing or sitting, regular exercise, and weight loss if overweight or obesity is present. Good skin hygiene is recommended
Treatment with diuretic drugs may help to eliminate excess fluid. These drugs increase the excretion of sodium and water through the kidneys. Diuretic treatment plays a key role in the treatment of heart failure where edema due to the retention of sodium and water is often a prominent symptom.
Using compression stockings and elevating the legs whenever possible is helpful. The stockings apply the greatest amount of pressure at the ankles and the pressure gradually decreases up the leg. This helps to pump blood back through the veins.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

Just my two cents worth. I was starting to get edema in my legs a few years ago, when I went on long haul flights. After I went low carb/high fat diet 5 years ago, I completely stopped getting edema even on long haul flights. I learnt from Dr Jay Wortman that on this diet the kidneys do not retain sodium like they do on a high carb diet.
I continue to have no problem with fluid retention at all. I am a 58 years old female. I am so glad I can travel without that issue. Now all I need is shorter legs when I am on these airplanes as I am 6 foot tall.
I suffered from terrible edema for decades, starting with my first pregnancy at 23, I had pre-eclamsia with that pregnancy and was on partial bedrest with my other two. As time went on, the swelling in my legs would reach as high as my thighs and I would walk for miles in a desperate attempt at relief.
Three years ago I adopted a ketogenic diet and the very first thing that happened was that the edema went away and never came back, 14 lbs that first week. Not during travel and not during the hormonal ups and downs of peri-menopause.
I have no varicose veins, no cellulite, and only 3 small spider veins.
An LCHF diet is a FAR more nature treatment than any of those listed here, not to mention all of the other health benefits. I only wish I had known about all of this in my 20s, my pregnancies would have been much easier and healthier.
Thanks for sharing very useful information with us.