Estimated reading time: 5 minutes
Elevated LDL-cholesterol (LDL-C) is common among people who adopt a low-carb, high-fat (LCHF) lifestyle. That’s why many physicians and nutritionists remain doubtful when it comes to LCHF, despite overwhelming evidence that such a dietary approach improves several other lipid parameters, usually leads to weight loss and positively affects glucose metabolism.
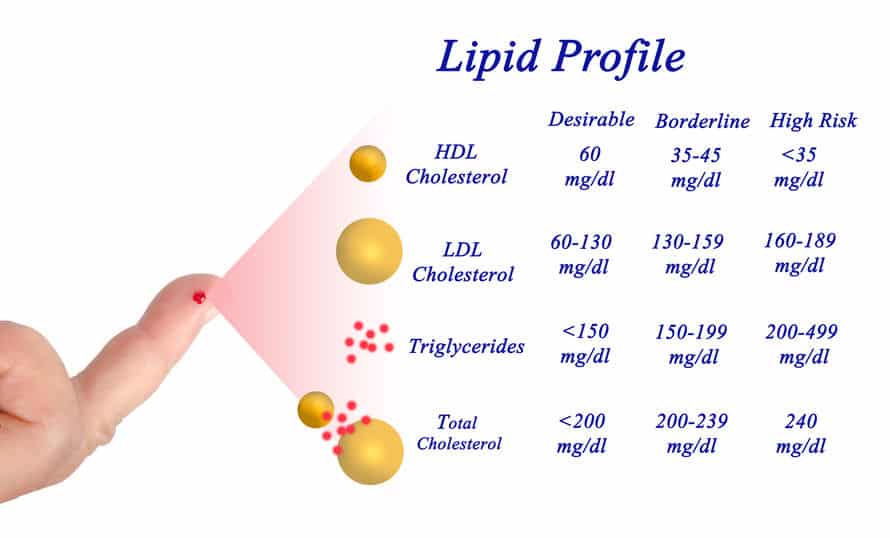
Several studies have shown that LDL-C constitutes a major risk factor for the development of atherosclerotic cardiovascular disease (1). Lowering LDL-C is considered a major target for reducing risk. The American College of Cardiology and the American Heart Associated advocate statin treatment for individuals with LDL-C above 190 mg/dL (4.9 mmol/L).
However, LDL-C is not a reliable risk marker for everyone. The main reason is that it is usually not measured in the laboratory. Although direct measurements are available, they are seldom performed due to costs. A standard lipid profile measures total cholesterol, triglycerides (TG)(2), and HDL-cholesterol (HDL-C)(3). LDL-C is indirectly estimated from these variables.
The bulk of cholesterol in the blood is carried by three lipoproteins, LDL, HDL and very low-density lipoprotein (VLDL). Other lipoproteins carry a negligible amount. Hence, if we subtract the cholesterol carried by HDL and VLDL from the total cholesterol, we will have an estimation of LDL-C. HDL-C is available from the standard lipid panel, so that’s not a problem. But, how can we estimate VLDL-C?
VLDL is an important carrier for TG’s in the blood. Although it also carries cholesterol, it is usually classified as a TG-rich lipoprotein. The ratio of the mass of TG to that of cholesterol in VLDL appears to be relatively constant and about 5:1 in healthy subjects.
So, if we subtract the HDL-C mass and 1/5 of the TG mass from the total cholesterol we will have an estimation of LDL-C. This is the Friedewald equation (4), named after William Friedewald, an American scientist and former professor of public health. This equation has been used for decades around the world to calculate LDL-C.
The Friedewald equation is used to estimate LDL-cholesterol (LDL-C)
If mg/dL is the unit (like in the United States) the formula looks like this:
LDL cholesterol = [Total cholesterol] – [HDL cholesterol] – [TG]/5
If mmol/L is the unit (like in Australia, Canada, and Europe) the formula looks like this:
LDL cholesterol = [Total cholesterol] – [HDL cholesterol] – [TG]/2.2
The Drawbacks of Calculating LDL-cholesterol
The major drawback of using the Friedewald formula to calculate LDL-C has to do with the assumption that the ratio of TG to cholesterol in VLDL is always the same which is not the case. LDL-C will be underestimated if the ratio of TG’s to cholesterol is higher than 5, and overestimated if it is lower than 5.
Following a fatty meal, blood levels of TG’s will rise. However, raised blood TG following a meal is caused by chylomicrons produced in the intestine, whereas elevated fasting levels are due to VLDL produced from TG’s in the liver. Chylomicrons disappear from the circulation soon after the TG’s have been delivered to the tissues. Therefore, using the Friedewald formula to calculate LDL-C is only applicable when chylomicrons are not detectable, and all the TG’s are being carried by VLDL. Hence, a fasting blood sample is necessary
The Friedewald equation is not applicable when TG’s are high. A recent study even suggested that the Friedewald equation tends to underestimate LDL-C among people with low LDL-C if triglyceride levels are moderately elevated (≥ 150 mg/dl) (6).
At present, only TG concentration higher than 400 mg/dL (4.5 mmol/L) is considered a limiting factor for the application of routine Friedewald equation. However, the fact that low TG levels may overestimate LDL-C also needs to be highlighted, not least because this may have practical implications for the growing number of people who adopt an LCHF lifestyle.
Introducing the Iranian Equation to Calculate LDL-Cholesterol
In a paper published 2001, Wang and colleagues described a patient with a low TG value of approximately 50 mg/dL, a high cholesterol level, and a discrepant LDL-C level (7). The LDL-C level using the Friedewald calculation turned out to be much higher than the LDL-C level using direct measurement. The authors suggested for the first time that in the presence of low TG and high cholesterol levels, the LDL-C level should be measured directly instead of using the Friedewald calculation.
These results were later confirmed in a paper published 2008 by Iranian investigators showing that with low concentrations of TG, the Friedwald equation may overestimate LDL-C to such a degree that may affect the clinical decision-making (8)
The Iranian investigators suggested a different equation for calculating LDL-C
If mg/dL is the unit (like in the United States) the formula looks like this:
LDL cholesterol =
[Total cholesterol]/1.19 +TG/1.9 – [HDL cholesterol]/1.1 – 38
If mmol/L is the unit (like in Australia, Canada, and Europe) the formula looks like this:
LDL cholesterol =
[Total cholesterol]/1.19 +TG/0.81 – [HDL cholesterol]/1.1 – 0.98
The investigators concluded that when using the unmodified Friedewald equation, low serum TG may positively affect the LDL-C calculation and to correct this error, the LDL-C level should either be directly measured or be adjusted by a modified formula.
This could have practical implications for people who follow an LCHF lifestyle which is fairly common nowadays. One of the first thing that happens during carbohydrate restriction is that blood levels of TG drop, often dramatically. Let’s take a real-life example.
A 47 year old man who adopted an LCHF lifestyle 6 months ago has
- Total cholesterol: 293 mg/dL (7.6 mmol/L)
- HDL-C: 60 mg/dL (1.5 mmol/L)
- TG: 70 mg/dL (0.8 mmol/L)
- Calculated LDL-C is 219 mg/dL (5,7 mmol/L) according to the Friedwald formula
- Calculated LDL-C is 190 mg/dL (4.9 mmol/L) according to the Iranian formula
That’s a fairly big difference isn’t it?
So, one of the reasons LDL-C is elevated on an LCHF diet may be that the Friedewald equation overestimates LDL-C when TG’s are low.

Why not just use Non HDL-C? Subtract HDL-C fom TC and you get a value that’s of use. Nothing fancy requiring additional tests.
BTW – regarding your example of the 47 year old man – no matter which measurement you use his LDL-C is very high.
Hi Charles
Agree with you on Non HDL-C.
https://www.docsopinion.com/health-and-nutrition/lipids/non-hdl-cholesterol-non-hdl-c/
A cheap and simple risk marker. And you don’t even need a fasting blood sample.
Very high, but Wang et al state that “Our patient was a 63-year-old man in good health”.
Further to that, they state
We, therefore, measured the LDL-C values on the same specimen using the direct method and obtained a normal value of 126 mg/dL! This value was further confirmed by the agarose electrophoretic method (130 mg/dL) and was also substantiated by a normal apolipoprotein B level of 116 mg/dL (60–130 mg/dL).
Remember that LDL and non-HDL-C, however calculated or measured, are intended as proxys for ApoB.
Would the 47 year old have ApoB outside this range? Maybe not, but if so, the difference is unlikely to be great.
Furthermore, the low TG/HDL ratio predicts that the atherogenic index of the LDL/ApoB is as low as possible.
For example,
The logarithm of the triglyceride/HDL-cholesterol ratio is related to the history of cardiovascular disease in patients with familial hypercholesterolemia.
https://www.ncbi.nlm.nih.gov/pubmed/22119890
George may I ask you a question regarding Cholesterolosis, fatty liver, leaky gut and what diet could be the best to shrink or get rid of cholesterol polyps in my gallbladder, Ive tried keto, Mcdougall, vegan, paleo but still have them, I figured that apart from diet I lose weight by exercising and practise IF, I thought that by reducing my feeding window to 6hrs and fasting for 18hrs then by about 15hrs Glycogen stores would have depleted and my body would start burning fat as its fuel but more importantly from the fatty liver and the process of auto-phagy could ‘munch’ those polyps, not sure if serrapeptase or selenium or other substances could shrink them.
During the day I drink tumeric tea or other herb teas like ginger/mint/milk thistle in order to keep my gallbladder moving bile and avoid bile stasis or saturation of bile/cholesterol in my gallbladder and drink lots of water during the day whilst fasting to keep bile fluid as well.
Forgive me I dont know where I could have asked this question and so I asked here, sorry if I annoyed you are anything like that its just that you seem so knowledgeable that I asked.
Hi Calegero,
this is well outside my experience, and I hope you have properly diagnosed and discussed this condition with your doctors.
Gall bladder operations do not seem to stop most people eating well – my mum had hers out years ago and says that except for the immediate post-op period it has never restricted what she can eat.
As a general point, the proper formation of bile acids and salts from cholesterol requires a few specific nutrients – these include glycine, taurine, and magnesium, and the long-chain PUFAs AA, DHA and EPA.
e.g. https://www.ncbi.nlm.nih.gov/pubmed/10652991
The more bile acids and salts you produce from cholesterol, the harder it should be for the cholesterol itself to form stones or polyps.
If you want to discuss this further, comment on my blog
https://hopefulgeranium.blogspot.co.nz/
Thankyou George,
Yes, I have been seeing my GP here in London, UK, was actually diagnosed in Wales two years ago with Cholesterolosis, I get ultrasound scans every 6 months to make sure the polyps haven’t reached the 1cm mark as they can become malignant if they reach 1cm or more.
Im not sure blog post to post on, should I just choose one that discusses fatty liver?
See you there 🙂
Hi Dr. Sigurdsson,
This post (and your blog in general) is incredibly eye-opening and well-written! I would love your thoughts on my pretty weird lipid panel if you could spare a few moments.
I am a fourth year American medical student trying to get all my health-related things in order before I disappear into the black hole of residency. One of these things is figuring out if I should be on statins. My cholesterol has been high for my entire life (not sure of exact numbers, but I think LDL >160 since I was 11 or 12). I’m going to get the genetic workup for FH, but the diagnosis doesn’t seem like a great explanation because I have no family history of early heart disease and neither I nor anyone in my family have xanthomas, corneal arcus etc.
My lipid panel a few months ago was:
Total: 290
Trig: 54
HDL: 91
VLDL: 11
LDL: 188 (Friedwald) — or 152! (Iranian)
LDL/HDL: 2.1
I am an otherwise healthy 28 year old woman — normal BMI, baseline blood pressure ~100/60, A1C 4.9, very active. My diet is, I guess fairly low carb in comparison to most Americans, but I eat lots of veggies including some starchy ones and am not a fanatic about avoiding sugar and grains, although they aren’t large parts of my diet. I take fish oil but am very hesitant to go on high-dose statins for life, which is what my cardiologist is really pushing. He also wants me to cut out eggs and basically all saturated fat, which will be a big dietary change for me. I could probably stand to eat less cheese but I’m hesitant to become essentially pescatarian, which is what he wants.
My current feeling is that if I do have an FH-type genetic defect, statins and aggressive dietary changes will be warranted. But if not, I think my astronomical HDL, low triglycerides, and low A1C suggest I’m doing most things right, metabolically speaking. Am I thinking about this right? Or should I go along with the statins either way and try to bring my LDL to a less scary number? And if I do go on statins, is it really necessary to cut out eggs and meat?
Thank you so much for your help!
Liz
Thanks for sharing this. I’ve been LCHF for 2.5 years. Total cholesterol 7.6 mmol/l, HDL-C 2.9 mmol/l, Trigs 0.7 mmol/l and LDL-C (Friedewald calculation) 4.4 mmol/l. Just calculated using the modified equation and it’s 0.8 mol/l lower at 3.6 mmol/l. I wasn’t concerned anyway as Trig/HDL ratio = 0.24.
When I refused statins for my calculated LDL of 210, HDL of 94, TG of 55 my doc decided to do a direct measurement of LDL. Came out 154. He still wants me on statins, but I declined given no history of cardiac disease and all ratios looking good. Now I understand why the calculated and direct were so different – thanks!
It’s really academic and out of date to even talk about LDL-C. Just go straight to NMR and check LDL-P. If that’s high then you probably have a problem. Multiply your goal LDL-C by 10 and that’s the goal LDL-p (roughly). I get all the talk about how this is an anti inflammatory diet and all the improved other parameters which is all really great for sure; but in the end I’m not willing to go off the ranch and tolerate a high LDL-P. All the lipidologists (Dr Dayspring e.g) I’ve read who understand keto still say numbers count. Maybe your LDL particles are big and ‘fluffy’, but high numbers are still high numbers. People with high LDL from familial hyperlipidemia still get disproportionate amounts of atherosclerotic vascular disease.
I don’t advise anyone over 40 to risk vascular disease and tolerate a super high LDL-P. That’s just reckless IMO. Educate yourself. This is new territory.
Hi Ted
I agree that LDL-P can certainly provide important information.
https://www.docsopinion.com/health-and-nutrition/lipids/ldl-p/
However, the method is not widely available.
Apolipoprotein B (ApoB) also reflects the number of atherogenic particles (rather than the cholesterol mass) but it’s not widely available either.
https://www.docsopinion.com/health-and-nutrition/lipids/apolipoprotein-b-apob/
It’s actually the insulin level that is more important as insulin drives the disease process, while the particles and other plaque building substances are kindling their business in the back seat.
High insulin and high ldlp are an issue, but again, atherosclerosis is not a single or even two bullet issue, but it really takes a village to cause the damage.
Almost forgot. Insulin is an anti-Statin as insulin ramps up cholesterol production. So lchf should lower cholesterol but in a good many cases it does not. These are the peeps we need to look at closer and figure out if they are truly at risk, or are we just being tricked by the tests again?
The problem is one of cost – a subsidised health care system such as we have in New Zealand will only provide standard lipid panels (HDL, total C, TG, calculated LDL) for primary prevention.
So we need to make the most of this, by using fasting TG/HDL to predict particle size and TG to choose LDL proxy calculation method.
While insulin increases the production of cholesterol (the molecule), and upregulates the mevalonate pathway in vascular endothelial cells, it can also increase clearance of ApoCIII bearing particles.
TG/HDL always correlates with 2-hour insulin, and can be taken as a decent proxy when insulin can’t be measured directly.
https://profgrant.com/2016/12/01/the-importance-of-the-fasting-tghdl-ratio/
The Iranian calculation is calibrated in populations with high total-C. Someone with normal total-C and low TGs may need a different calculation again.
Martin etc all proposed a novel calculation for LDL-C in 2013 that accounts for inter-individual variability in VLDL for LDL calculation. This may be a better option than the Friedewald equation in certain cases (I.e. low LDL levels sought after with genetic dyslipidemias or patients on lipid-lowering therapy). https://jamanetwork.com/journals/jama/fullarticle/1779534?resultclick=3.
This may not be relevant for LCHF dieters, but still an important move forward in LDL calculation.
I agree and this is important to apprehend. Basically all the available data on LDL-C as a risk marker is based on Friedwald calculations. So, data on the relationship between directly measured LDL-C and cardiovascular risk is not really available.
If Ldl-C and Ldl-p are discordant then use ldl-p but if they are
concordant then you can use ldl-c according from what I have read and I believe Dr dayspring says the same thing??I have been getting the NMR lopoprofile test for 2 years now and every time my ldl-c went up my ldl-p went up and every time my ldl-c went down my ldl-p went down…I eat very healthy because I have heart disease…latest test ldl-c was 73 and ldl-p was 722.Before that 84 and 848 before that 95 and 958 and the first time ldl-c 155 ldlp-1650.Small dense was 855 now 167…apo-b was 95 now 63 apo-a1 was 120 now 167,…and yes i eat animal protein and no STATINS.
ClinicalChemist makes a good logical argument in their last paragraph here, this is conceptually correct.
However it is perhaps answerable – if risk calculations from Friedewald LDL-C were relatively exact, consistent between populations, and minimally affected by other measures, it would be right to continue using them in all cases, but as of course they are not, clinicians will seek more information, and the alternative calculations can provide reassurance in circumstances where it may not be reasonable to follow guidelines if this could mean prescribing unnecessary medication.
That’s right George. Although we’ve relied on the Friedwald equation for many years, knowing the true LDL-C must be what we’re after. Therefore it is important to know the limitations of the Friedwald approach and when it is likely to mislead us.
I’m having familiar hypercholesterolemia (heterozygous) and since you were pointing out that high dosage of statins may increase the risk for diabetes I was working hard on reducing my dosage. Now I’m down to 20 mg Atorvastatin/10 mg Ezetimibe and LDL/HDL and Triglycerides are great.
My choice:
– four to five times exercise a week (endurance and weight-lifting)
– a mild form of LCHF (I skipped the Skaldeman ratio)
– intermittent fasting (5:2)
I’ve tried LCHF first in an 8-weeks setting without fasting and was suprised about the results – my LDL was pushed down to 51 mg/dl, HDL went up above 60 and total cholesterol was about 120. I never had such great results and I’m taking statins since 2009!
Trying it with the same dosage and “normal” meals pushed triglycerides up to 150 and LDL to 96.
At least under statin treatment I can’t see a negative impact of LCHF-like diets – might be different for untreated people but in my case it was an eye-opening experiment. Sugars and flour are the real threats in my opinion!
So my total cholesterol was 420,Hdl was 60,LDL 328,triglycerides 151
My Doctor upped my Lipator to 40 mgs.I have lost 60 lbs. Doing keto diet.Any suggestions on the Lipa tor should I stop it,I am also on savella 200mg. Which has been known to elevate women’s cholesterol in women age 50 to 59..