Estimated reading time: 8 minutes
Growing up and living with the diet-heart hypothesis through my professional career has been a remarkable experience.
I was lucky. My mentors were great. I went to all the big cardiology conferences. I read the best books and I learned from the great masters.
Early on, I was taught the fairly well established relationship between blood cholesterol and coronary heart disease.
The message to our patients was very clear; lowering blood cholesterol is the main target. It can be achieved by reducing fat intake, avoiding dietary cholesterol and replacing saturated fat with polyunsaturated fatty acids and complex carbohydrates.
But I wonder why we didn’t ask more questions. Why didn’t we request more data? Cardiologists are very research-oriented and usually claim scientific proof for everything.
Was our belief in the diet-heart hypothesis so strong that we didn’t need studies to confirm that our dietary advice would be of benefit?
The Warning Signs
Of course, there were those who warned that we might be on the wrong trail.
In 1977, Dr. George V. Mann wrote in The New England Journal of Medicine: “A GENERATION of research on the diet-heart question has ended in disarray (1)”. Mann later wrote a book called Coronary Heart Disease: The Dietary Sense and Nonsense – An Evaluation by Scientists. His book understandably evoked mixed emotions (2).
Mann’s book contained the views of members of the Veritas Society, who in November 1991 met to voice their objections to the diet-heart hypothesis, which they believed was “based upon fragile and selected data.” The society called “for a return to scientific and informational honesty.”
Mann wrote in the preface to his book that “the regulatory agencies have been derelict in their duties, allowing fraudulent health claims to continue in food and drug advertising.”
In 2001, journalist Gary Taubes highlighted the soft science behind the dietary fat hypothesis in a famous article published in Science (3).
US journalist Nina Teicholz took these arguments a step further in her book The Big Fat Surprise that was published 2014.
Uffe Ravnskog, a Danish doctor, has fought relentlessly for decades to convince the medical society that we were wrong about dietary fats and their proposed role in heart disease.
Of course, many physicians still believe that a low-fat diet is the best food choice, and the most effective one to reduce the risk of cardiovascular disease.
In fact, vegetarians appear to have low risk of cardiovascular disease. But nobody has proved it’s because they eat less fat and cholesterol. Vegetarians eat less sugar as well. Antioxidant compounds and polyphenols in fruit and vegetables—such as vitamin C, carotenoids, and flavonoids may be beneficial. Fruit and vegetables are good sources of magnesium and potassium, which have been inversely associated with mortality in previous studies.
In 1988 a small paper reported findings from a group of seven patients with food allergy and elevated serum cholesterol levels who were forced to follow a diet in which most of the calories came from beef fat (4). Their diets contained no sucrose, milk, or grains. During the study, their cholesterol and triglyceride levels decreased significantly, and levels of HDL cholesterol increased.
The investigators wrote:
These findings raise an interesting question: are elevated serum cholesterol levels caused in part not by eating animal fat (an extremely “old food”), but by some factor in grains, sucrose, or milk (“new foods”) that interferes with cholesterol metabolism?
Sadly, our delusive focus on dietary cholesterol and saturated fat dismisses a huge amount of scientific data suggesting that the effects of diet on cardiovascular health are mediated through many biologic pathways other than cholesterol, including oxidative stress, low-grade inflammation, insulin sensitivity, endothelial dysfunction and blood clotting mechanisms.
By claiming the diet-heart hypothesis is the sole key to our understanding of the role of diet in heart disease, medical professionals like myself have kept the lid on proper understanding of the role of the relationship between dietary factors and cardiovascular disease.
In his book, Pure, White and Deadly, published in 1972, UK doctor John Yudkin wrote:
One of my main reasons for taking up research in this field was that I became more and more uneasy about the prevalent simplistic view of how people get coronary disease – the idea that it is just a matter of cholesterol levels in the blood. This idea is now so firmly held by so very many people that they end up believing that anything that increases cholesterol in the blood is likely to cause coronary disease, anything that reduces cholesterol helps to prevent the disease or even cure it, and anything that does not invariably increase the cholesterol in the blood must have nothing whatever to do with the cause of heart disease. – I know I’m biased, but this picture – in my view a rather naive one, has hindered a proper understanding of its prevention.
Sugar and Heart Disease
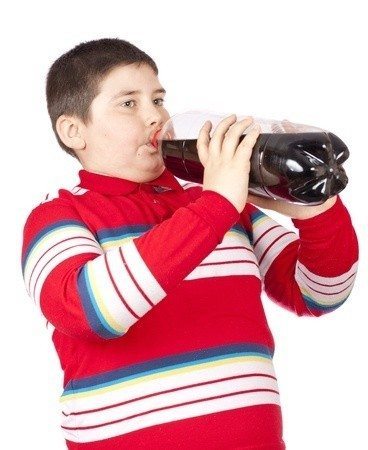
Lately, we’ve seen epidemiological data suggesting that increased intake of sugar-sweetened beverages increases the risk for metabolic syndrome, type 2 diabetes, coronary heart disease, and stroke (5).
Human intervention studies have showed accumulation of fat in the liver, muscle, and the visceral fat depot induced by sugar sweetened beverages. Most of the studies support the fact that fructose is the main driver of these metabolic aberrations presumably by inducing lipid synthesis and fat release from the liver (6).
Interestingly, Ancel Keys, the father of the dietary-heart hypothesis found an association between sucrose consumption and the risk of coronary heart disease but didn’t think it was an issue. As highlighted in Robert H. Lustig’s book Fat Chance, he believed high sucrose consumption was only a surrogate that correlated with high intake of saturated fat.
Key’s wrote:
The fact that the incidence rate of coronary heart disease was significantly correlated with the average percentage of calories from sucrose in the diets is explained by the intercorrelation of sucrose with saturated fat.
A very recent paper published in the American Journal of Clinical Nutrition by US investigators addresses the link between sugar intake and cardiovascular risk factors (8). The study tested the effects of consuming beverages sweetened with different doses of high fructose corn syrup on blood lipids and uric acid in 187 adult participants.
The study found that blood levels of LDL-cholesterol, non-HDL cholesterol, and apolipoprotein B, postprandial triglycerides apoCIII and uric acid increased in a dose-dependent manner within two weeks following consumption of different doses of high-fructose corn syrup.
The authors believe their findings provide a plausible mechanistic link to the increased risk of death from cardiovascular disease associated with increased intake of added sugar.
In Pure White and Deadly, John Yudkin describes findings from several laboratories clearly showing that sugar in the diet increases plasma levels of cholesterol and triglycerides. Sugar consumption was also associated with a rise in insulin levels and increased stickiness of platelets that may increase the risk of blood clotting.
A very interesting finding from Yudkin’s studies was that a quarter or a third of their study subjects showed a special sensitivity to sugar while the remainder did not. These individuals showed more rise in insulin levels and they put on more weight than the others.
Yudkin suggested that it might be useful to screen for individuals who were “sucrose sensitive” because they might by at increased risk of coronary heart disease.
Another mechanism whereby sugar consumption may increase the risk of cardiovascular disease is through its effects on blood pressure.
It is well known that high blood pressure increases the risk for cardiovascular disease. Yudkin describes a study performed by Richard Ahrens from the US, who carried out an experiment with young men who were given diets containing varying amounts of sugar. Their blood pressure rose proportionally to the quantity of sugar in the diet.
Decades later, a meta-analysis of randomized controlled trials showed that high intake of sugar is associated with elevated blood pressure (9).
In a 2014 review paper in Open Heart BMJ Journals, the authors highlight that recommendations to reduce consumption of processed foods in order to reduce hypertension are highly appropriate and advisable. However, they propose that the benefits of such recommendations might have less to do with sodium and more to do with highly-refined carbohydrates (10).
The Bottom Line
High intake of sugar and refined carbohydrates is associated with increased risk of diabetes, metabolic syndrome, non-alcoholic fatty liver disease, lipid disorders and high blood pressure.
Recent findings showing an association between sugar consumption, fructose in particular, and the risk of cardiovascular disease suggest that we have to broaden our perspective in order to understand the relationship between dietary choices and cardiovascular disease.
For years, our overemphasis on the role of dietary fats and blood cholesterol has blurred our understanding of a multifactorial and much more complicated association between diet and heart disease.
Understandably, the medical community and public health authorities may have a hard time admitting their ingenuousness. Furthermore, considering all the commercial interests involved it may be guileless to think that honesty and belief in the scientific method will prevail.
However, let us remember Winston Churchill’s words
To improve is to change; to be perfect is to change often
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.


Your article is confusing and maybe misleading. You identify
sugars as the culprit and then don’t distinguish between the various types-
sucrose, high fructose corn syrup (HFCS), and fructose in fruit. You say that
vegetarians eat more fruit (and vegetables) and less sugar. You don’t explain
why the fruit isn’t bad. Your hypothesis that vegetarians eat less sugar (and
processed grains for that matter) is without any factual basis. From what I
see, vegetarians eat lots of grains, often processed grains with added sugars,
and added sugars to healthy vegetable-based products that would be bitter
without it. Sugared health drinks also. How about granola? Have you read the
labels on granola (fat, sugar, salt)? Do you think canned beans are any
different? Look at a can of Hanover kidney beans. Corn syrup ,salt, and sugar.
Oops. I think your theory just fell apart.
You infer that heart health is not about cholesterol (other than “good”
cholesterol) levels, but rather about other factors, like sugar consumption.
Then you go on to say that sugars increase risk by raising cholesterol levels.
Huh?
“The study found that blood levels of LDL-cholesterol,
non-HDL cholesterol, and apolipoprotein B, postprandial triglycerides apoCIII
and uric acid increased in a dose-dependent manner within two weeks following
consumption of different doses of high-fructose corn syrup.”
There are people that are running around saying that LDL
levels don’t matter. That would seem to be a mistake. Maybe some tolerate high
levels better because of the “quality” of their HDLs or some other factor. Maybe it’s a combination of factors like that
and ability to “tolerate” various sugars.
You’ve convinced me that most doctors are followers. People
that are great at memorizing things, but not at critical thinking. I just don’t
think your theories are any better.
As I have read, 75% of “bad” cholesterol is produced by the
liver. 25% comes from diet. So you can
move your cholesterol levels, just not as much as you can by affecting the
amount your body produces. You did say vegetarians have lower cholesterol
levels because they eat no meat. But I believe they eat as many sugars as the
meat eaters, just more hidden sugars.
So I think it would be a good idea to clarify all this and
be brave enough to provide an example of a diet that is healthiest. Okay, we
can all read labels and avoid processed foods (to include grains) that include
sugars (does it matter where the sugars came from?) and other additives. We
know to restrict calories. But how much
(if any) meat should we eat? What percentage of calories from fruit is okay?
What percentage of carbohydrates? Is it about eating vegetables that aren’t
canned (added salt, corn syrup, and
sugar)? What about potatoes and pastas? How much? What kinds? All of the theories and “reasons” are nice,
but people need fact based answers. Something they can apply. What should we be eating? In what percentages?
If we do that and are healthier, we don’t need to know the chemistry behind it.
I’m going shopping tonight. Let me know.
Thanks.
Thanks for your comment Pete.
Your criticism of my article mainly relates to issues I did not write. I won’t respond tho those because it’s out of my scope.
However, for the sake of clarification, I feel I must respond to a couple of issues
The studies I refer to and my article in general relates to added sugar. That is mostly sucrose (glucose and fructose) or fructose or high fructose corn syrup. Obviously I’m not talking about fruit unless they are fruit products with added sugar such as fruit juice for example.
You wrote
“Oops. I think your theory just fell apart.
You infer that heart health is not about cholesterol (other than “good”
cholesterol) levels, but rather about other factors, like sugar consumption.
Then you go on to say that sugars increase risk by raising cholesterol levels.
Huh?”
But I never did infer that heart health is not about cholesterol. I may have inferred that heart health is not only about cholesterol. I hope you understand the difference.
And I certainly implied that there are other factors that matter as well. So, my belief that high amounts of added sugar may increase the risk of heart disease does not mean cholesterol and other lipids don’t have anything to do with it. Why would I believe that nature is that simple?
Axel wrote – “Obviously I’m not talking about fruit unless they are fruit products with added sugar such as fruit juice for example.”
So why does fruit get a free pass? Fructose is fructose, whether it is delivered via HFCS or in a slice of watermelon. Fruit as we know it today didn’t exist until man crossbred it for size and sweetness. I don’t think it wise to assume something is healthy (or at least not unhealthy) just because it’s grown in the dirt. Particularly when we get fruit year round rather than just when it was in season like when I was a kid.
Bob
The fact that fruit is not dealt with in this particular blog post doesn’t necessarily imply that it gets a free pass.
Maybe a subject of another article?
Of course it should get a free pass, unless you’re talking about something like eating dozens of bananas a day.
Fruit gets a free pass because the fiber it contains slows the rate at which the fructose gets metabolized. In addition to this the amount of fructose in a serving of fruit is considerably less and would require overeating a very high amount to reach harmful levels.
Fiber? Really?
Seems to me that whole wheat has a decent amount of fiber but I know that whole wheat spikes blood sugar just as high and just as long as white flour and is just as detrimental. Regardless of how long that fructose rush from a piece of fruit takes to get to the liver it still has to be metabolized by the liver.
And what do you mean by “considerably less”? Are you saying there’s a safe level of consumption for a toxin like fructose? I think I’d like to see a citation for this.
There’s no data to indicate that consumption of fruits is harmful but plenty of data to indicate that it’s beneficial. Furthermore, if you argue that fructose is a toxin regardless of intake and carrier food, the burden of proof rests on your shoulders.
Plenty of data showing it’s beneficial? Really? I notice you didn’t provide any. And compared to what? Sounds like a lot of observational data where it’s compared to a much worse diet. Am I close?
Are you really saying that your liver can differentiate between fructose that was ingested as sugar or fructose that was ingested as fruit? Fructose is fructose, the chemical composition is the same and the source matters not at all. The only thing that matters is the individual’s ability to metabolize it without ill effects. If you have Non-alcoholic fatty liver disease or a host of other conditions I would think that removing fructose from your diet entirely would be prudent.
Have you ever wondered why it’s your liver that metabolizes fructose and not some other pathway? We have an elegant and efficient way to metabolize fat and protein and a much less effective pathway to deal with glucose but fructose is shunted to the liver where it’s dealt with along with all of the other substances your body deems to be toxic. I wonder why that is…
“I notice you didn’t provide any.”
No, I didn’t. Surely that means it doesn’t exist, right? 🙂
“And compared to what? Sounds like a lot of observational data where it’s compared to a much worse diet. Am I close?”
Well, d’uh. In case you didn’t know, everything in diet & studies of their effect has a point of comparison against which it is judged. E.g. fat and lipid levels: their effect is pitted against that of carbs. Or diets: the point of comparison is the current diet (Western) of the participants. Was this somehow news to you? If so, what’s the matter with it?
And are we going to hear banalities like “correlation-isn’t-causation” next?
“Are you really saying that your liver can differentiate between fructose that was ingested as sugar or fructose that was ingested as fruit?”
Check my message. I presume/hope you can read.
“If you have Non-alcoholic fatty liver disease or a host of other conditions I would think that removing fructose from your diet entirely would be prudent.”
Yes, I bet you would, wouldn’t you. Now you’ll just have to show that eliminating fruit from the diets of those in such conditions is beneficial to them. 1-2-3-go!
“Have you ever wondered why it’s your liver that metabolizes fructose and not some other pathway?”
Not really. Have you – or any other low carber/paleoista/whatever ever wondered that e.g. dietary safa is simply NOT needed: there is no such thing as an essential saturated fatty acid. Why should we eat it then?
Or better even: have you paused to think that these questions of yours are simply irrelevant & a smoke screen to avoid dealing with the current understanding of healthy components of any given diet which don’t fit your dogmatic way of thinking? 🙂
So basically you agree with everything I said except that you’re never are curious about why the various pathways that exist in our bodies are there. That’s some deep thinking.
No essential saturated fatty acid – if that’s your logic the perhaps you can explain why there’s no essential carbohydrates.
So … basically you didn’t understand anything I said.
Nor do you understand humor, based on your final sentence.
Nice going Bob.
The difference between bread and fruit is that the carbohydrate in bread is glucose, which is known to spike insulin by a considerable amount, where as fruit contains mostly fructose which has no insulin response.
What I mean by “considerably less” is that in moderation the the benefits that come along with fruits may, in certain cases, outweigh the harmful effects of the fructose. Apologies for the poor choice of words I used.
Fruit gets a free pass because the fructose is mitigated by high fiber.
Doc, is high LDL (300) always bad? Does it make a difference if it is from a high fat diet or if it is from some other disorder? (see my previous post on LDL tripling on a high fat diet.) IN the studies that show high LDL is associated with heart disease, what are the numbers? IE does everyone with high LDL get heart disease? Out of 100 people with LDL of 300, do all of them die early or do some live long? I am not interested in ‘increased risk by x%; I don’t know what that means?
If 1 out a 100 people with low LDL get heart disease and high LDL doubles the risk, then only 2 of a 100 get heart disease. I can live with that. But if 1 in 100 with low LDL get heart disease and 99 of 100 with high LDL get it, that is a different story.
I only have high LDL on a high fat diet. I get lean, strong and can go long times without eating on high fat
Thanks for the comment Joe.
These issues have been discussed in several comment forums on my blog. You will probably find most of it here https://www.docsopinion.com/health-and-nutrition/lipids/ldl-p/
I took a look – said that ApoB / ApoA1 ratio is more important that just ApoB. But did not say what the ratio should be.
Joe
The preferable ApoB/ApoA ratio is <0.6 for women and <0.7 for men.
High fat/ketogenic diet appears to raise LDL cholesterol quite much in some individuals. Nobody really know what this means in terms of risk.
Here's a good discussion on the subject https://www.lowcarbdietitian.com/blog/lipid-changes-on-a-very-low-carb-ketogenic-diet-my-own-experience
ouch – on a low carb/high fat diet with my high cholesterol high (385) and LDL was high (283) my apoB was 184 (bad) and my apoA1 was 199 (good) – my ratio was .92, bad. After a month on a low fat, high complex carb diet my cholesterol dropped (196) and my apoB dropped 122 (lower but still high) my apoA1 got worse (126) so the ratio got worse (.96)
Also my inflammation went through the roof. crp from 32 to 12.
I never had a cholesterol or inflammation problem before – this is very recent. I am starting to wonder if it is connected to a recent change in exercise. I always, always exercised very hard every darn day. I switched to a ‘high intensity, less frequent, much, much shorter workout nd had a few issues.
The workout is slow reps (which are much more stressful on muscles but easier on joints), no rest between sets, basics only, one set of each muscle group and each exercise to absolute failure and beyond (continuing to push in an isometric fashion after failure)
I get nauseous, dry mouth, difficulty swallowing, clogged ears, and chills afterward. Its great!
But I also got rosacea on my nose. After being told we don’t know the cause, I stumbled across an article saying it is sometimes a histamine intolerance. After looking up histamine, I now think they are related. The workout send my body into panic, stress and inflammation. I cut down the exercises and increased the frequency and the symptoms, including the rosacea, lessened – the infrequent (once a week) caused me to regress in overall endurance and the reaction is more violent with more time off. increasing frequency leaves me more resistant to the systemic fatigue and I don’t get nauseous, or chills. The nose zits practically left.
I wonder if this stress is causing these other problems?
Typo, that was 2 crp on high fat to 12 on high carb.
It’s either damaging or not-so-damaging, depending on the context (overall AR). Considering that it (often) takes place in the context of weight loss is a pretty good sign that the diet sucks.
Of course you can be on a HFLC diet and not get increase in LDL. You just have to eat better food.
Pete,
It is good that you are thinking and it is also good that you challenge Axel upon certain points.
Sugar is neither ‘good’ nor ‘bad’ per se. It is natures way that certain safeguards tend to accompany sugar found in natural foods. it is very mucg the modern way that those certain natural safeguards have been eroded by compromise that assocaites with modern methods and process.
I would guard against assuming that all fruits are high in fructose or that fructose is the only sugar to be found in fruits, and I would guard against thinking fructose is ‘better’ than glucose or other glucose derived polysaccharides.
The general assumption within cardiology is that cholesterol is a concentration dependent atherogen, and that cholesterol alone can induce tissue changes through being present in blood in (supposed) higher concentrations. In actuality cholesterol is not a concentration dependent atherogen, while certain oxides of cholesterol may have atherogenic properties that rise with their rising concentrations.
The evolutionary approach, one which attaches upstream accounts to cholesterol, and the biochemical and endocrinological approach which gives an account for how cholesterol derived biochemicals can account for gender and reproductive process in animals (but not in plants) points the way that cholesterol has pivotal importance to the biology of animals but precious little significance to the biology of plants (despite sharing a biosynthetic pathway in common). The pivotal importance of cholesterol, once appreciated, strongly discourages faithful inclination to think cholesterol is the killer.
Cholesterol does not kill mammals. Cholesterol is the significant member of the significant family of sterols that makes possible the kind of cells that make up the kind of tissues that make animals a real and biological possibility and that differentiate animals from mere vegetables.
To improve is to change. To change is to improve. To be reductionist is to learn.
To be sufficiently inclusive and holistic in outlook, concern, and interest is to take any reductionist learning and subject it to scrutiny. The measure of scrutiny that reductionist gains are subjected to that sieves the wheat from chaff. Separating chaff from chaff improves the quality, and improved quailty helps changing opinions trend in accordance with facts. only when opinions are trending in accordance with facts (when viewed as inclusively and holistically as is humanly possible) can we hope they are improving while trending.
Perfection is hard to attain. But if improvements are trending with facts, with as many facts as is possible, then improvements are a trend in the general direction towards perfection.
I openly wish the opinions held within cardiology would trend a bit quicker.
When I read Axel I observe his opinions are trending, and to his credit his opinions are trending just a bit quicker than is normal within cardiology. He has to be careful. If his opinions trend too quickly he will become an outcast in his field irrespective of how sound, correct, holistic, and evidence based they are. I mean, just consider how much of an improvement Galileo’s trending opinions were, yet look at how he was treated by those whose opinions did not trend either so well or so fast.
i drive a truck for a living. I have can my opinions upon cholesterol, upon CAD, upon cardiology, cardiologists in general, and upon Axel, trend in any way I like and as fast as I like. And I like Axel, for he is adventurous, courageous, and prepared to openly discuss matter of great importance. In the least there are occasions when his mind and opinions are prepared to trend. That distinguishes him from many of his colleagues.
I am confused about Milk being a new food??? (the land of milk and honey??)
“A very interesting finding from Yudkin’s studies was that a quarter or a third of their study subjects showed a special sensitivity to sugar while the remainder did not. These individuals showed more rise in insulin levels and they put on more weight than the others.”
One of the favorite ploys of apologists for the sugar industry is to note that normal weight individuals, on average, consume more sugar than fat people. From that they conclude that sugar is not “uniquely fattening.” Says Bill Shrapnel, “The latest WHO report is notable for what it doesn’t say about sugar. It doesn’t say sugar is addictive, toxic, uniquely fattening, or that it gives you fatty liver, heart disease or diabetes. That’s because these are all just myths peddled by attention-seeking, non-nutritionists to boost their celebrity, sell books and make money.” https://scepticalnutritionist.com.au/?p=1844
Note, the two thirds to three quarters of Yudkin’s study subjects who did not show a “special sensitivity to sugar” would respond to high sugar intake in this way: “The difference in plasma lipid response of healthy normolipemic subjects to different types of carbohydrate was found to be minimal. Five healthy subjects were found to maintain their serum lipid levels within the normal range despite relatively high sugar content of their “home diet.” The students did not develop a significant hyperlipemia even after their average dietary sugar content was raised to 285-300 g/day for 3 weeks. This amount of dietary sugar constituted about 30-40% of their daily caloric intake. Feeding experiments suggested that it was necessary to raise dietary carbohydrate to 85-90% of the total calories, and to supply the major proportion of it as sugars, before significant degrees of hyperglycerdemia could be induced in subjects who do not have disturbances in carbohydrate and glyceride metabolism.” https://ajcn.nutrition.org/content/20/2/116.full.pdf+html
Critics of the low-carb movement use the same sort of reasoning to argue that high carbohydrate intake is not uniquely fattening. “The mechanism of production of primary hyperglyceridemia has not been satisfactorily defined. Primary hyperglyceridemia is currently differentiated into the “fat-induced,” the “carbohydrate-induced,” and the “mixed” forms, according to the manner in which the patient’s plasma triglyceride level changes with varying proportions of fats and carbohydrates in the diet. A number of investigators have shown that hyperglyceridemia can be induced in normal subjects and greatly exaggerated in hyperglyceridemic patients by high carbohydrate diets. However, it is well-known that people of the underdeveloped areas of the world, subsisting on high carbohydrate diets, apparently do not develop hyperglyceridemia.” https://annals.org/article.aspx?articleid=680091
Axel,
An excellent post, an excellent analysis, and an excellent choice of quote upon which to end. However, have you come around to reading into the biological effects of the several cholesterol oxides. As contributing editors Peng and Morin contributed an excellent book upon the subject (1991) which would still stand as an introduction to the subject matter, and a springboard from which to seek out more contemporaneous mention in literature.
There are 49 identified and naturally arising alternate cholesterol oxides. These seem to have some involvement in signalling and status management. Ergo they work like simple hormones. That the oxides of cholesterol have the potential to have influence akin to recognised hormones ought not to surprise interested parties because a family of hormones are derived from cholesterol. These are the steroidal family of hormones and these have bearing upon gender and sex in mammals especially, but across many other animals too.
Then cholesterol belongs to a ‘family’ itself. It is one of around 200 sterols. In this family are phytosterols and zoosterols. Cholesterol is the prominent zoosterol. Cholesterol has a provenance, indeed all sterols do, since they are derivative of mevalonic acid, and mevalonic acid is derivative of glucose. Come to this with the open mind of an evolutionary biologist and realise that glucose is the product of the earliest of chloroplastic life-forms then it is a short step to realise that natures capacity to produce mevalonic acid cannot pre-date chloroplastic capacity to photosynthesise glucose.
Ergo, sometimes after the first ever molecule of glucose there must have been a great evolutionary step in biochemical possibilities that gave rise to first ever molecule of mevalonic acid. only some time after that could the fort ever sterol have been synthesised. That cholesterol was not the first sterol to emerge within this 200 strong family is indicated by its place in biology as a zoosterol, and by the overriding energetics of the great food chain. Plants must have proliferated first because they altered atmospheric conditions and enriched atmospheric oxygen while assimilating energy from the sun. In the extended food chain and through their capacity to fashion basic hydrocarbons its the chloroplasts that provide the energy and conditions for animals to eat. CO2 becomes O2 only for the O2 to be converted back to CO2.
So, the family of sterols was once a family of just one, but that diversified (evolved) over time to a family numbering 200. The phytosterols were needed first and the zoosterols can only have arrived (evolved) later. Without a highly lipophilic zoosterol (such as cholesterol) cells with lipid membranes could not have been possible, because biology strongly implies cholesterol makes lipid membranes and lipid transport possible. Cholesterol is derived from the same acetyly and mevalonate pathway that gives rise to sterols in plants. It does strongly seem that biochemical sophistication in chloroplasts was a long evolutionary trend that paved the way for the eventual emergence of cells with lipid membranes held together by the suitably lipophilic sterol we call cholesterol.
Phytosterols and zoosterols share similar provenance (from the acetyl and mevalonate pathway that is common to both) and yet plants have no need of zoosterols and animals have next to no need of the phytosterols. Fascinating.
If you come at coronary artery disease from a cytological perspective, with knowledge of the distinctions between cholesterol and its several oxides, then the orthodox view in cardiology begins to look weak. The advance of therosclerosis requires alterations to cytological expression that cholesterol per se does not induce. However certain cholesterol oxides seem to influence certain aspect of cell expression in certain types of cell, and this altered expression does account for some of the changes observed with the advance of atherosclerosis.
It would appear, for the above and for other indications (homocysteine), that oxidative stress may feed the advance of atherosclerosis and coronary artery disease. It might also be the case that certain hormonal states gives rise to the promotion of oxidative stress that might then go on to generate proliferation of certain cholesterol oxides, and believe this or not certain cholesterol oxides may be factorial in ramping up the biosynthesis of cholesterol in certain cells such as hepatocytes and macrophages.
The risk factor approach merely serves to disguise how little is actually known and it does little to dispel confusion.
On the other hand curiosity that begins from a cytological approach encourages interest in certain cholesterol oxides and oxidative stress, and this in turns leads into curiosity for the proliferation of oxidising factors and/or the paucity of antioxidant availability. Follow this lead and two generalsistaions begin to seem promising. Oxidative stress is a lifestyle issue gives rise to shifts endocrinological balance and thus promotes oxidative stress, while dietary factors and lifestyle factors can account for relative paucity of antioxidant availability. Oxidative stress is axial, Axel.
With methylation being an antioxidant pathway, perhaps the leading antioxidant pathway, and with homocysteine being a strong indicator of methylation stress and of CAD then it would seem hypercortisolemia, hyperinsulinemia, gluconeogenesis, and hyperlipidemia would each be bedfellows under certain circumstances, and those same circumstances might be ones that contribute to oxidative stress, while demand for, and poor supply of key B group vitamins undermines capacity to metabolise and mitigate potent oxidising factors via methyl group donation.
The risk factors are several. Highly glycemic foodstuffs, sugar included, are just one risk factor driving endocrinologic imbalance that drives oxidative stress that results in compromised cytological expression that in turn accounts for the tissue changes observed in the advance of atherosclerosis.
I do highly recommend Peng and Morin on Cholesterol Oxides.
I do highly recommend you take up with interest in 25-hdroxycholesterol as a signalling factor having influence over cholesterol synthesis (as an agonist ramping up cholesterol synthesis) and also in sulphated 25-hydroxycholesterol as having contrasting influence over cholesterol synthesis (as an antagonist reigning it back).
7-Ketocheolesterol looks a bit suspect as does cholestane-triol.
Thank You Christopher Plummer. I learned much from your article. Your take on this subject is much appreciated! You opened some wonderful doors in my mind.
Thanks for this great summary!
I’ve experienced the great success of a grain- and sugar-drained diet by myself: I’m having fam. hypercholesterolemia (Fredriockson IIa) and learned by a set of diet changes that a severe sugar- and grain-reduction accompagnied with a high rise of fat intake resulted in a better LDL-reduction than doubeling the atorvastatin dosage!
Now let’s see how C-RP will do…next Check is in June – after cutting the atorvastatin dosage from 40 to 20 as reaction to you latest post regarding the risk of diabetes….
So, thanks for your input, it helps me a lot!
Max
“Understandably, the medical community and public health authorities may have a hard time admitting their ingenuousness. Furthermore, considering all the commercial interests involved it may be guileless to think that honesty and belief in the scientific method will prevail.”
This is the reason I fear for the health of western nations. Too much to lose in changing dietary advice. I’ve read we’ll be allowed to eat cholesterol now, well, most of us. My guess is that there will be an insidious release of ‘new’ information over prolonged periods of time and eventually the general populace will be told about the toxicity of consuming high carbohydrate, high calorie diets and highly processed foods.
This doesn’t serve us well. I believe the science is out there but hasn’t been permitted much light.
Thanks so much for your posts, doc.
Iam not saying this based on any scientific study.. But purely out of my observation.
Here in India we have a fair bunch of vegetarians, who are culturally born and raised in such traditions due to cultural and/or religious reasons. Talking specifically about South india where I come from, we have a great deal of heart patients out here. And vegetarians in here use sugar and dairy very liberally in their diet. Tea and coffee with sugar multiple times a day is norm.. Not to mention our love affair with sweet snacks.
I can understand things might be different in west where people take this as a life style and would be more health conscious than the indians who are born in to such a culture.
And I think we South Indians have the highest concentration of diabetic patients in India (if not in the world).. We those who live the state of kerala usually even refer to diabetics as ‘sugar’ , yes.. the exact english word sugar.. Like saying ” he has sugar “.
Thanks Ashkar.
Very interesting. Are there any theories regarding the high incidence of diabetes among the South Indians?
What’s the prevalence of obesity?
What about rice consumption? A meta-anaysis from 2012 showed an association between whithe rice consumption and type-2 diabetes. https://www.ncbi.nlm.nih.gov/pubmed/22422870
Theories in here mostly revolve around sugar.. I do not usually see doctors advicing patients regarding rice consumption much.. (My parents are doctors, Iam not)
But some do advice to reduce rice consumption aftrer one turns diabetic though ! Its mostly just insulin injuctions and some advices regarding sugar and fruits for most of the part. But havent heard anyone talk about limiting rice consumption as part of a measure to limit chances of turning diabetic. Not even as one of the probable cause. Its not even a talking point.
Rice, legumes and vegetables are part of staple diet. Legumes and vegetables actually form as side dishes. Or as dosas (crepe) and such. Refined wheat consumption is increasing year by year.
(Rice and side dishes, mainly at noon: Something like this: https://upload.wikimedia.org/wikipedia/commons/a/a6/A-_SOUTH_INDIAN_FOOD_AFTER_SERVING.jpg )
Obesity is skyrocketting every year, dealing obesity has become a very profitable industry.
Its very high in vegetarian population. Non alcoholic Beer belly is common among vegetarian adults.
Ashkar
Very informative and interesting.
Appreciate your input.
You are welcome.. Looking forward for more informative posts..
Ashker, I have also read your observations elsewhere. Railway doctors observed greater heart disease and diabetes in the vegetarian areas. They thought animal fat was protective. In the west though, it’s taken for granted that that is not the case. A lot of what is passed on to us as nutritional science is anything but.
None of this seems to square with me and from what I read, some paleo folks whose LDL skyrocketed on paleo.
I went on a three-year, very high fat, very low carb diet, before which my LDL was 105 on a balanced diet of about 1/3 each of F, P and C. My LDL went to 305. I switched to a very low fat diet of mostly starchy carbs from rice and sweet potatoes, and fruit, and protein for a month and my LDL went to 120.
I have a complete Boston Heart breakdown of particle size etc for both tests and need a good low carb doc to explain to me either: that I need some carbs and should not be eating so much saturated fat or explain why my 300 LDL is OK. My GP is an Onrnish guy. By my blood work he seems to be right.
I have been on a balanced diet of F, P and C again and plan on another test. I expect results somewhere between the two. Interestingly my glucose and insulin levels did not go up on the low fat diet.
Axel, when you write things like
“By claiming the diet-heart hypothesis is the sole key to our understanding of the role of diet in heart disease, medical professionals like myself have kept the lid on proper understanding of the role of the relationship between dietary factors and cardiovascular disease.”
shouldn’t you be ashamed of constructing a straw man? When was the last time anyone suggested that restricting sugar intake WASN’T beneficial?
And “delusive focus” on saturated fat? Err, since when did it stop increasing LDL levels and impairing HDL functionality? Or are you still having problems understanding the results of several meta-analysis showing IMPROVEMENT in both risk markers and hard end-points when safa –> pufa? And what’s even more confusing is that you while you blurt out something like that, you offer data which is LESS convincing than what there is for dietary fats & risk of CVD to make your case for sugar??!!? Does “false dichotomy” ring a bell?
Seriously: what is so damn impossible about understanding that BOTH the intake of safa and sugar had better be minimal – and that this issue is solved without too much fuss when adhering to a healthy diet?
I’m glad yo agree about added sugar.
However, I don’t think you’ll find any textbook of cardiology discussing the role of added sugar in the pathogenesis of cardiovascular disease. But you will certainly find a lot on dietary fats and how we should eat or not eat them depending on how they affect our lipid levels.
Look at the European Guidelines on cardiovascular disease prevention in clinical practice (version 2012) https://eurheartj.oxfordjournals.org/content/early/2012/05/02/eurheartj.ehs092
There’s your traditional discussion on SFA’s vs PUFA’S and recommendations about limiting saturated fat. However, the guidelines state that “after >40 years of research, the impact of saturated fatty acid intake on the occurrence of CVD is still debated. Recently, a meta-analysis of cohort studies did not show an increase in the relative risk for CHD or CVD with higher intake of saturated fat…”
The guidelines mention soft drinks are as a possible risk factor. for obesity, type 2 diabetes and cardiovascular disease. But there are no recommendations regarding sugar sweeetened beverages an added sugar in general.
“However, I don’t think you’ll find any textbook of cardiology discussing the role of added sugar in the pathogenesis of cardiovascular disease.”
Perhaps that’s because it’s rather a matter of etiology, just like safa intake? Both have an effect on lipid levels not per se but the key point is WHAT they replace in diet: both unsaturated fats and fiber-rich foods lower cholesterol as compared to sugar & safa. You CAN of course have both added sugar and safa in your diet, provided that the big picture is in order.
“But you will certainly find a lot on dietary fats and how we should eat or not eat them depending on how they affect our lipid levels.”
Because the meta-analyses of e.g. metabolic ward studies clearly indicate their effect? 🙂
“Look at the European Guidelines on cardiovascular disease prevention in clinical practice (version 2012)”
I am well aware of what they say on the topic. Let’s have the rest of the paragraph here, shall we? It says:
“… although there may be several methodological issues explaining this null finding.280 A number of studies adjusted the effect of saturated fatty acids on CVD for serum cholesterol levels—an example of overadjustment. Another important aspect is by which nutrient saturated fatty acids are replaced. The evidence from epidemiological, clinical, and mechanistic studies is consistent in finding that the risk of CHD is reduced by 2–3% when 1% of energy intake from saturated fatty acids is replaced with polyunsaturated fatty acids.270 The same has not been clearly shown for the replacement with carbohydrates and monounsaturated fatty acids. Therefore, lowering saturated fatty acid intake to a maximum of 10% of energy by replacing it with polyunsaturated fatty acids remains important in dietary prevention of CVD.”
You knew this. Why the false dichotomy then? Why the misleading use of “delusive”, as the shortcomings of e.g. many fat exhange studies/fat reduction studies have been clearly discussed here in this very blog several times over? Why?
“But there are no recommendations regarding sugar sweeetened beverages an added sugar in general.”
As you surely know, there isn’t that much convincing evidence that sugar is a major direct risk factor (and not indirect via met.syndrome/DM2) – no RCT’s with hard end points, for instance. In addition, the guidelines have recommendations concerning the form of carbs in diet. – no added sugar there, as you can read yourself. And the guidelines do discuss the association between soft drinks and increased risk of CHD. And they discuss entire dietary patterns, too.
So the problem is …? If you have data indicating a particular amount of added sugar (% of tot. E) should be recommended, do show it. To me the key message of the guidelines is pretty clear.
Mie
“As you surely know, there isn’t that much convincing evidence that sugar is a major direct risk factor (and not indirect via met.syndrome/DM2) – no RCT’s with hard end points, for instance.”
In fact, I think there is a lot of evidence that that added sugar is a major risk factor for metabolic syndrome, insulin resistance, DM, hypertension, NAFLD and cardiovascular disease (it doesn’t matter whether it’s direct or indirect). I thought we agreed on that. You said: “what is so damn impossible about understanding that BOTH the intake of safa and sugar had better be minimal?”
Considering the hard end-points. Where are those when it comes to dietary fats?
“So the problem is …? If you have data indicating a particular amount of added sugar (% of tot. E) should be recommended, do show it.”
You know I can’t show such data.
But, where’s the data sowing that keeping SFA’s below 10% (or 7% for that matter) of total calories consumed is beneficial? Who invented this figure? What’s the evidence behind it?
Why do we need hard end-points when it comes to added sugar but not for recommendations that already made it into the guidelines?
“In fact, I think there is a lot of evidence that that added sugar is a major risk factor for metabolic syndrome, insulin resistance, DM, hypertension, NAFLD and cardiovascular disease (it doesn’t matter whether it’s direct or indirect). I thought we agreed on that.”
For most of these, yes. CVD? I wouldn’t call it a major direct risk factor, based on the evidence at hand. Whether it being direct or indirect risk factor matters or not … well, I suppose it really doesn’t. At least not in a larger context. Anyway, consuming a large amount of added sugar is detrimental to health at any rate.
“Where are those when it comes to dietary fats?”
Err, did you read the quote?
… “the risk of CHD is reduced by 2–3% when 1% of energy intake from saturated fatty acids is replaced with polyunsaturated fatty acids.”
“But, where’s the data sowing that keeping SFA’s below 10% (or 7% for that matter) of total calories consumed is beneficial? Who invented this figure? What’s the evidence behind it?”
There are plenty of studies, including meta-analyses like this
https://www.bmj.com/content/314/7074/112
showing what reductions in safa intake do to LDL levels – and hence to CHD risk.
But in fact, I agree with you in that figures such as these are more or less not needed – provided that the focus is on whole dietary patterns as it should be. Of course, the key message is about controlling your lipid levels: for some it requires reductions ALSO in safa intake all the way down to that particular amount of safa, for others more – or less.
“Why do we need hard end-points when it comes to added sugar but not for recommendations that already made it into the guidelines?”
As you can see, quite a few of the dietary elements discussed have either end-point data or extensive epidemiological data to accompany them. Including soft drinks. So …? But yes, of course it’d be better if there were enough quality studies for all the given elements.
So … Care to finally explain that “delusive” comment?
I’ll correct myself and lend (somewhat preliminary) support to sugar being a direct risk factor in atherosclerosis via lipid level changes. I checked an earlier discussion on the role of sugar in CVD (among other things) at Reijo’s blog because I had a vague flashback of something that might be related to the topic at hand.
https://www.pronutritionist.net/sokerin-terveyshaitat-suhteessa-tyydyttyneeseen-rasvaan/
Now, that’s in Finnish so the interesting part is here
https://www.ncbi.nlm.nih.gov/pubmed/23471231
Both glucose and fructose have detrimental effects, glucose in terms of chylomicron remnants (ApoB-48) and fructose in LDL etc. (ApoB-100).
Ther’s also the very recent AJCN paper I cited in my blog article https://ajcn.nutrition.org/content/early/2015/04/22/ajcn.114.100461.abstract
BTW Axel, I’m still waiting for your answer to the questions below:
“Why the false dichotomy then? Why the misleading use of “delusive”, as the shortcomings of e.g. many fat exhange studies/fat reduction studies have been clearly discussed here in this very blog several times over? Why?”
Oh, I almost forgot: for some reason, you listed three people (Taubes, Teicholz and Ravnskov) who’ve been perhaps most active in contributing to the onslaught of nonsense and plain BS in the world of “internet experts” (sic). Without mentioning that their contributions haven’t “exactly” stood up to scrutiny.
Care to explain why?
Mie.
I listed Mann and Yudkin as well.
I know you don’t hold Taubes, Teicholz and Ravnskog in high regard and I’m sure some of their contributions “haven’t exactly stood up to scrutiny”.
However, they’ve had the courage to to challenge current concepts regarding the role of diet in heart disease and obesity. I consider that ti be important because I think these concepts deserve to be challenged.
If they’ve managed to get people like you get up on your feed and shout, they’ve certainly achieved something.
“However, they’ve had the courage to to challenge current concepts regarding the role of diet in heart disease and obesity. I consider that ti be important because I think these concepts deserve to be challenged.”
Ah, the “courage”. Indeed, I suppose you will then applaud e.g. Peter Duisburg for “courage” in HIV denialism, too?
Or could it be that challenging current concepts should be done SCIENTIFICALLY? Don’t know about you, but I’d sure as hell prefer that. 🙂
“If they’ve managed to get people like you get up on your feet shouting, they’ve certainly achieved something.”
Oh yes, in the same vein as any other Internet trolls.
Axel, have you actually read their work? Or critiques of it?
“Understandably, the medical community and public health authorities may have a hard time admitting their ingenuousness. Furthermore, considering all the commercial interests involved it may be guileless to think that honesty and belief in the scientific method will prevail.”
You probably meant “disingenousness” (if not, that first sentence makes very little sense). Too bad that
a) dietary advice has always changed to reflect the change in scientific understanding – and continues to do so
and
b) “commercial interests” haven’t exactly blurred our understanding of the dangers of high intake of sugar as dietary guidelines have advised against it for … gee, I dunno … decades?
Mie. “Ingenuousness”, in the context I was using the word refers to naivety. But I guess the word “disingenousness” also fit swell. Appreciate the tip.
“In 1988 a small paper reported findings from a group of seven patients with food allergy and elevated serum cholesterol levels who were forced to follow a diet in which most of the calories came from beef fat (4). Their diets contained no sucrose, milk, or grains. During the study, their cholesterol and triglyceride levels decreased significantly, and levels of HDL cholesterol increased.”
That study had 7 people. That’s not even remotely worth mentioning. And you presented it in an entirely misleading way. Not very professional of you.
It might also be considered unprofessional not to mention these results because they illustrate the individual variation in the effects of different macronutrients on blood lipids.
Interestingly recent data from the large Pure study showed that higher carbohydrate intake was associated with a lipid profile characterized by lower HDL-C and ApoA levels, leading to higher Cholesterol/HDL-cholesterol and ApoB/ApoA ratios and higher TGs.
https://www.docsopinion.com/2016/08/01/carbohydrate-fat-and-lipids/
Arslan Library is the ultimate source to Download Free Medical Books in PDF. This website has been designed especially for Medical Students & Doctors and it holds a vast range of Medical Books. Visit our website and Download Free Medical Books. https://arslanlibrary.com/category/all-free-medical-books/