Estimated reading time: 8 minutes
Obesity is a condition characterized by excessive accumulation of body fat and increased body weight.
Scientific studies have revealed that obesity is associated with negative effects on health and reduced life expectancy.

Obesity is most often defined as a body mass index (BMI) above 30. High BMI is associated with increased risk of high blood pressure, lipid disorders, type 2 diabetes and cardiovascular disease.
However, the definition of BMI has several problems. It doesn’t account for different body frames, and it doesn’t differentiate between muscle and fat.
Many individuals with high BMI don’t have the metabolic abnormalities associated with obesity and will not develop the typical complications of this disorder.
Furthermore, many normal weight individuals suffer from the same metabolic abnormalities that are usually associated with obesity. These subjects are often defined as metabolically obese, normal-weight (MONW) (1).
Visceral Obesity
Many studies have shown that body shape and the regional distribution of fat may be more important for health than the total amount of body fat. Most importantly, it has been shown that the accumulation of fat around the internal organs may play a key role. This phenomenon is often termed visceral obesity.

The term visceral obesity defines excessive fat accumulation around the organs within the abdominal cavity.
The terms central or abdominal obesity, or belly fat, describe fat accumulation in the upper part of the body and don’t differentiate between visceral or subcutaneous fat accumulation. Usually, belly fat is a combination of both.
Evidence that visceral fat tissue is more damaging to health than subcutaneous abdominal fat is rapidly emerging. Research suggests that obese individuals with excess visceral obesity have a higher risk of diabetes, lipid disorders, and cardiovascular disease than those with less visceral fat accumulation (2).
Central obesity is defined as waist circumference
≥ 40 inches or 102 cm in males and
≥ 35 inches or 89 cm in females
History
In 1947, Professor Jean Vague from the University of Marseille, was the first to recognize that the regional distribution of body fat was a more important predictor of risk and metabolic abnormalities than excess fatness in general (3).
Vague defined two different body shapes. Android obesity or apple shape refers to the accumulation of fat in the upper body area. Gynoid obesity or pear shape refers to the accumulation of fat on the hips and thighs. The latter is more common among women than men.
Although Vague’s ideas were initially met with skepticism, they were later confirmed by scientific studies.
In 1984, the results of a large Swedish epidemiological study showed that an increased abdominal waistline among middle-aged men and women was strongly predictive of higher risk of coronary heart disease later in life (4,5). Later these same investigators showed that central obesity was strongly associated with increased risk of diabetes.
Central Obesity and Health
Studies have shown that the accumulation of belly fat is associated with several disease conditions such as type 2 diabetes, lipid disorders, high blood pressure, cardiovascular disease and some types of cancer. Most of these studies have used waist circumference to define central obesity although some have directly assessed visceral fat by using modern imaging techniques.
Insulin Resistance and Type 2 Diabetes
Insulin resistance is defined as a diminished response to a given concentration of insulin and is associated with increased risk of type 2 diabetes.
Insulin resistance and type 2 diabetes are key features among people with central obesity. In fact, central obesity appears to be a better predictor of type 2 diabetes than general obesity assessed by BMI (6).
Lipid Disorders
Lipid abnormalities commonly associated with central obesity include high levels of triglycerides and low levels of HDL-cholesterol. Consequently, the triglyceride/HDL cholesterol ratio is elevated.
People with central obesity often have normal total cholesterol and relatively normal levels of LDL-cholesterol. However, they often have high number of LDL particles that can be measured by raised levels of LDL-P and Apolipoprotein B. A high number of LDL-particles is associated with increased risk of atherosclerosis and cardiovascular risk in general.
Central obesity is often associated with small and dense LDL particles. Small LDL particles bind weakly with LDL-receptors making their clearance from the circulation less efficient. Therefore, small LDL particles are likely to circulate for a longer time, increasing the total number of LDL particles available. Furthermore, insulin resistance worsens the clearance of LDL particles from the circulation (7).
The combination of high triglycerides, low HDL cholesterol, and small, dense LDL particles, often termed the “atherogenic lipid triad”, is strongly associated with the risk of cardiovascular disease.
High Blood Pressure
High blood pressure (hypertension) is a well-known risk factor for heart disease and stroke. Hypertension is more common in obese people than normal weight individuals.
Studies have found that central obesity assessed by waist circumference is associated with increased risk of hypertension (8).
Cardiovascular Disease
Central obesity is a predictor of cardiovascular disease and mortality, independent of traditional risk factors and BMI (9). Thus, abdominal obesity appears to be a stronger risk factor for cardiovascular disease than general obesity in itself.
Interestingly, the Nurses’ Health Study found the cardiovascular risk of overweight/obese women without central obesity was similar to that of normal weight women with central obesity (10).
The large INTERHEART study indicated that central obesity was a stronger predictor of heart attack (myocardial infarction) than general obesity assessed by BMI.
Cancer
Epidemiological data have showed an association between obesity assessed by BMI and increased risk of several types of cancer (11).
Similar data also indicate that central obesity may be associated with increased risk of cancer of the colon and rectum, breast cancer in women, prostate cancer in men, and cancer of the esophagus.
Why Do We Accumulate Belly Fat?
The mechanisms behind central obesity are complicated. Why do some individuals accumulate fat within the abdominal cavity while others don’t?
Age and gender clearly play a role. Young individuals are more likely to store excess fat under their skin (subcutaneous fat) than around the organs of the abdominal cavity.
The ratio of visceral to subcutaneous abdominal fat tends to increase with age. Furthermore, women tend to have much higher proportion of subcutaneous than visceral fat compared with men of same age.
Men are much more likely to accumulate fat in the upper body, whereas women often accumulate fat in the lower parts of the body, on the hips and thighs.
Sex hormones appear to play a role. Men with low testosterone levels tend to have more central obesity than those with normal levels. Estrogen treatment of female-to-male transsexuals appears to increase subcutaneous fat depots in all areas.
Studies have clearly shown aggregation of visceral obesity in some families (12). Thus, genetic factors appear to influence how much fat is stored under the skin compared with around the visceral organs.
Nutritional Factors
Very few studies have assessed nutritional factors that may underlie central obesity.
Recently published data from the PREDIMED study revealed that a Mediterranean diet supplemented with nuts was associated with less central obesity, lower triglyceride levels, less small and dense LDL particles and lower LDL particle number (13).
Consumption of sugar sweetened-beverages is associated with increased risk of obesity and type 2 diabetes. Intake of fructose raises triglyceride levels and blood sugar.
In fact, data suggests that the intake of fructose stimulates visceral fat accumulation more than the intake of other simple sugars (14).
Physical Inactivity
Although it has not been proven that a sedentary lifestyle predisposes to the accumulation of belly fat, there is evidence that regular exercise is associated with less central obesity.
A systematic review found that regular physical activity was associated with a marked reduction in central obesity, even in studies not reporting reductions in body weight (15).
Why Should We, and How Can We Lose Belly Fat?
The strong association between central obesity and diverse disease conditions suggests that avoiding the accumulation belly fat, or losing belly fat if present, may reduce risk and improve health.
Any intervention that will induce weight loss is likely to reduce belly fat.
In theory, weigh loss interventions that target visceral fat preferentially may improve health without the need for general weight loss. However, the principal finding of a recent review (16) was that there are no effective interventions available that target visceral fat preferentially.
So, if somebody claims that a certain approach will reduce belly fat more than other fat, you can be certain that this intervention is not supported by scientific evidence.
Restricting carbohydrates may help lower triglyceride levels. This may improve lipid profile by increasing LDL particle size, and reducing LDL particle number and apoliporotein B levels. In fact, the positive effects of dietary carbohydrate restriction in people with insulin resistance and type 2 diabetes may have been underestimated (17).
As mentioned previously, a Mediterranean-type diet may reduce belly fat and improve some of the metabolic abnormalities associated with central obesity.
Many experts believe that physical exercise is not effective when it comes to losing weight. However, failure to recognize the benefits of exercise, independent of weight loss, is misguided.
Obese individuals can improve their health without losing weight. In my opinion, regular physical exercise should play a key role for the treatment of central obesity.
Estimated reading time: 8 minutes
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

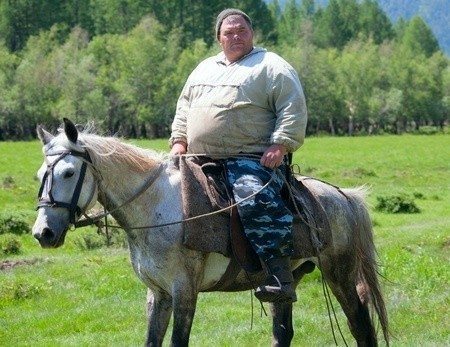
First thought I had was poor horse!
He is the only one without a choice, the rest of us need to pay attention.
Thanks so much for this comprehensive summation of the complexities of lipoproteins, CVD risk factors, diet and nutrition. From my own experience, I observed the effects of moderate refined carbohydrate restriction that resulted in a significant decrease in triglycerides and a significant increase in HDL-C.
Thanks for the comment.
I agree with you that carbohydrate restriction is often very effective in metabolic syndrome; when visceral obesity, insulin resistance, high triglycerides, low HDL-cholesterol and high LDL particle number cluster together….
Hi Axel,
Just want to say thanks for all your posts, excellent source of information and your patience with some of the trolls is admirable.
One question I would like to ask is have you any thoughts on the role of glycated LDL, there was a recent article (research paper) which discussed high blood glucose and the subsequent creation of glycated LDL which appeared to be ‘sticky’ and therefore more atherogeneric. Apologies for the school boy terminology.
Makes me think blood sugar control is such an important factor in cardio vascular health.
Thanks,
Bill.
Thanks Bill
In fact it’s possible that glycated LDL plays an important role in atherosclerosis, partcularily among diabetics. It has been shown that glycated LDL is more easily oxidated than native LDL. Oxidized LDL appears to be involved in atherosclerosis.
Keep in mind however that oxidized LDL is not found circulating in blood. LDL can’t be oxidized untill it enters the arterial wall. However, glycated LDL is found in blood.
It’s also of interest that small dense LDL is easily glycated, both among diabetes and non-diabetics. This may partly explain why small dense LDL particles appear more atherogenic than other particles.
The role of glycated LDL might explain why diabetics are much more prone to atherosclerotic cardiovascular disease than non-diabetics.
In terms of prevention or treatment, any food or supplement that reduces the glycation of LDL might be of interest.
Very interesting, would it be possible to describe what oxidizes the LDL when it enters the arterial wall? I have heard many times than oxidized LDL is one of the problems rather than just LDL.
Thanks,
Bill.
Scientists would do well to pay more attention to the bioactive properties of polyunsaturated fatty acids. Especially important are the impacts on appetite, metabolic activity, and fat storage patterns. This 2013 research may turn out to be a breakthrough in terms of our ability to understand some of the effects of excessive omega-6 intake. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3889814/
Dr. Joseph Hibbeln commented on this research in a 2013 interview entitled More “Vegetable” Oil? MORE Heart Deaths. Excerpts:
“Just as all polyunsaturates are not created equal, all high fat diets are not created equal. A good example of this is an animal study we did where we compared three high fat diets. All with 60% of calories from fat, in mice. We compared high fat diets that resembled the linoleic acid, Omega 6 intakes, comparable to the levels at the beginning of the century, which was about 1 percent of calories, and those high fat diets with 8 percent of calories, more similar to the amount of Omega 6 in the diet simply from soy oil in the U-S diet, today. Moving from 1% to 8% linoleic acid in the mouse diets, not only tripled the levels of arachidonic acids, but also tripled the levels of a critical derivative of arachidonic acids, which is an endogenous cannabinoid, which creates a similar affect to marijuana. So it’s the brains own marijuana like molecules, and we were able to triple the body’s marijuana like hormones, three times higher in the liver and about 20% higher in the brains just by altering the linoleic acid in those two high-fat diets. Normally those high fat diets used for mice in studies are composed of high linoleic acid, found in soybean oil. When we deleted that one single molecule, the Omega 6 fatty acid, we were able to obliterate the ability of a 60% high fat diet to induce obesity in the mice…And we did it also in diets that were 35% of calories from fat, and also diets that were 12% of calories from fat. We were able to induce obesity in low fat diets, in the mice, by changing the bioactive properties of the fat, not just that it was high fat and more calories.” https://www.meandmydiabetes.com/2013/03/10/vegetable-oil-associated-with-more-heart-deaths-nih-scientist-joe-hibbeln/
Axel,
good article. However, to provide some context to the reader, you could have pointed out that the highest CHD mortality ever measured was among Eastern Finns of the 1950s. Obesity, belly fat and diabetes where exceptionally rare within this post-war group of timbermen who had never ingested added transfats, coco-cola, french fries, pizza’s, etc as these food groups did not exist in the Eastern Finnish food supply at the time. There where no shortage of whole-milk, butter and other carbohydrate- poor foods. When the CHD mortality was at its peak in Iceland you can also by almost utmost certainly confirm to me that there no abundance of fat people in Iceland at the time.
Exactly Richard. The risk profile for heart disease has changed in the last fifty years as suggested here.
It seems that selenium deprivation (as commented by George Henderson) had a direct link to cardiovascular disease too.
Ive struggled with my weight since around the age of 18 (im now 25). I have to admit its my own fault – I made very unhealthy choices daily. I knew I was overweight and that I had a bit of a belly, but after measuring my waist (92cm) it was a shock to find out that Im considered centrally obese! For the last few years Ive been more physically active but I struggle with portion control and healthy eating a lot. Thus far I have not lost much weight and Ive only managed to maintain my overweight status. Im glad I havent gained but Im struggling to get healthy. I also have raised blood pressure. Im just unsure what avenue to turn to for help??
Thanks for another excellent explication of a complex subject Axel. The epidemiological and clinical trial evidence in favor of a Mediterranean style diet and regular moderate exercise is indisputable. No fads, just time-honored consumption of real minimally processed food and being physically active is what we all need to stay healthy.
I agree Barbara. It’s not complicated. But somewhere/somehow we seem to have wandered off the path…
Thank you for this informative article.
I’ve also read from other sources that recent studies show that increased level of the hormone adiponectin (produced by fat tissues) can help the body store excess fat in the subcutaneous area rather than the viscera, and that exercise is a potent stimulator of raising adiponectin levels.Subcutaneous fat is happy (safe) fat. Visceral fat is grumpy (dangerous) fat. This can explain why there are obese (like the sumo wrestlers) who maintain healthy lipid profiles despite of being fat. Please correct me Dr. Axel if I’m wrong. Always been a fan of your remarkable work. Regards.