Estimated reading time: 5 minutes
Data presented at the World Heart Federation’s World Congress of Cardiology & Cardiovascular Health 2016 (WCC 2016) in Mexico City may radically change our perspective on how carbohydrates and different types of fats affect blood cholesterol and other lipid biomarkers. The presentation was based on data from the Prospective Urban Rural Epidemiological (PURE) study. The data have not been published yet, and the results are only available in an abstract (1).
The study, presented by researchers from McMaster University, Hamilton, Canada, addresses how carbohydrate and fat intake affected blood lipid profiles in 145.000 individuals living in nineteen low- to high-income countries. The researchers conclude that the message to reduce the intake of saturated fats for the purpose of lowering cholesterol and thus decrease risk of cardiovascular disease may be misleading
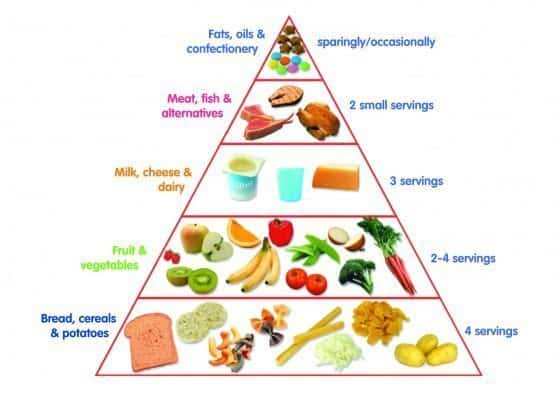
For decades, blood cholesterol was assumed to be a robust surrogate marker to predict the risk of heart disease. A reduction in saturated fats is recommended to reduce cholesterol levels, and carbohydrates are placed at the bottom of the food pyramid, mainly because they tend to lower cholesterol levels. Public health authorities have recommended that 60 percent of daily calories should come from carbohydrates.
However, the low-fat, high-carbohydrate approach has recently been challenged, and the authors of the recent study point out that there are no data from low and middle-income countries where more than 80 percent of cardiovascular disease occurs.
The PURE Data on Nutrition and Lipids
The goals of the study were to describe the association between nutrient intake and blood lipids and to examine the effect of iso-caloric replacement of nutrients on blood lipids.
The habitual food intake of 145,275 participants in 19 high, middle and low-income countries who were enrolled in the PURE study was prospectively measured using validated food frequency questionnaires.
The lipid biomarkers addressed in the study:
- Total cholesterol (TC)
- LDL cholesterol (LDL-C)
- HDL cholesterol (HDL-C)
- Triglycerides (TG)
- Apolipoprotein A (ApoA)
- Apolipoprotein B (ApoB)
The macronutrients addressed in the study:
- Carbohydrates
- Saturated fatty acids (SFA)
- Monounsaturated fatty acids (MUFA)
- Polyunsaturated fatty acids (PUFA)
Higher carbohydrate intake was associated with lower TC and LDL-C but also with lower HDL-C and ApoA levels, leading to higher TC/HDL-C and ApoB/ApoA ratios and higher TGs. The apoB/apoA ratio has repeatedly been shown to be a better marker of risk than lipids, lipoproteins and lipid ratios (2)
A higher intake of SFAs was associated with higher LDL-C and lower TG levels. Higher MUFA intake was associated with lower TC, LDL-C, and higher ApoA. Higher PUFA intake was associated with lower TC and LDL-C and paradoxically higher ApoB level.
Iso-caloric replacements of carbohydrates with SFAs increased TC by 3%, LDL-C by 5% and HDL-C by 1% and decreased TG by 5%. Replacement of carbohydrates with MUFA led to a 2% decrease in LDL-C, 3% decrease in TC/HDL-C ratio, and 1% decrease in ApoB/ApoA ratio. Replacing carbohydrates with PUFAs was associated with little change in lipid markers.
The authors concluded that higher carbohydrate intake has the most adverse impact on lipid profiles and replacing it with saturated fat improved HDL-C and TG and replacing it with MUFAs improved TC/HDL-C and ApoB/ApoA.
“These data from a large global study indicate that guidelines on dietary fats and carbohydrates require re-evaluation.”
The Bottom Line
Public health authorities, including the American Heart Association (AHA) and the World Health Organization (WHO) recommend that 60% of calories should come from carbohydrates and only 5% to 6% of calories from saturated fat.
In the above study, the only benefit of a high carbohydrate diet was a lowering of TC and LDL-C. However, the effect on other lipid biomarkers such as HDL-C, TG, and ApoB/ApoA ratio may be harmful.
A diet rich in SFAs raised TC and LDL-C but lowered TG while a diet rich in MUFAs improved all lipid biomarkers. A diet high in PUFAs had a mixed effect on lipid biomarkers.
The study suggests that placing carbohydrates at the bottom of the food pyramid based on their effect on blood cholesterol was a mistake. In fact, the data show that replacing dietary carbohydrates with different types of fat may improve lipid profile.
In an interview on Medscape, Dr. Mahshid Dehghan, the principal author of the abstract said (3):
To summarize our findings, the most adverse effect on blood lipids is from carbohydrates; the most benefit is from consumption of monounsaturated fatty acids; and the effect of saturated and polyunsaturated fatty acids are mixed. I believe this is a big message that we can give because we are confusing people with a low-fat diet and all the complications of total fat consumption, and WHO and AHA all suggest 55% to 60% of energy from carbohydrates.
Today, most experts agree that diets high in SFAs or refined carbohydrates are not be recommended for the prevention of heart disease. However, it appears that carbohydrates are likely to cause a greater metabolic damage than SFAs in the rapidly growing population of people with metabolic abnormalities associated with obesity and insulin resistance.
I assume we all agree that partially hydrogenated fats (trans-fats) should be avoided. However, the singular focus on reducing the intake of SFAs, and dietary fats in general, may have been counterproductive and promoted the rapidly growing popularity of refined carbohydrates. The nutritional data from the PURE study clearly suggest that it is time to shift our focus away from reducing fat in our diet towards reduced consumption of carbohydrates.


Hooray and about time! Ditch the starchy carbs. Eat the fat. Now please will you persuade Slimmimg World to stop encouraging low fat chemical filled rubbish and eating starchy carbs and to just eat the fat and stop starchy carb consumption? No pressure then ????????
Is there any distinction drawn in the study — Please excuse my inattention if I missed it, but I am still struggling with the various ‘threads’ in the whole picture! — between sugars and other carbohydrates? I suspect the reference to ‘refined’ carbohydrates (which I interpret as sugars? …as opposed to potatoes for example) may be the sort of distinction where my question is directed…?
Of course thats a very important question Don.
There is no distinction between refined vs. non-refined in the abstract. Hopefully we’ll get that when the paper is published.
According to Medscape, when the study was presented at the congress, “an audience member wanted to know if the study found any evidence of a shift to more processed foods, even in low- and middle-income countries. Dehghan replied that they did find this, adding that low-income families mostly consume refined carbohydrates (the worst kind) and don’t consume whole grains.”
Hi Axel, have you seen this new report from WHO (Mensink) of saturated fatty acids (compared with carbs and other nutrients) and effects on lipids? https://www.who.int/nutrition/publications/nutrientrequirements/sfa_systematic_review/en/ It’s a review of more than 90 trials, you should check it out.
Thanks Erik.
Appreciate it.
Looking forward to check it out.
Is it not so that saturated fat increases HDL? Is is also not so that satfat increases particle size? Is it not so that the place in the world with the highest satfat consumption (Gascony, Le Perigord, whatever you want to call it) has the lowest CHD in France, a country which shares with Japan, the lowest CHD rate in the world. Using these facts says that “Worse than Saturated Fat” is not appropriate in the heading. Worse implies that satfat is bad. The evidence is that it isn’t at all. Huge meta-analyses have concluded that there is not link. Can you explain your heading, Axel?
A valid point Garry
Maybe “High fat intake better than high carb for blood lipids” would have been better.
However, medical professionals tend to focus on LDL-C and LDL-C only. They see high fat (particularly saturated fat) as a bad thing for LDL-C.
In the recently published European guidelines on cardiovascular prevention these are the first two key messages in the chapter on lipid control:
-Elevated levels of plasma LDL-C are causal to atherosclerosis.
-Reduction of LDL-C decreases CV events.
Hence, everything that raises LDL-C is bad. Therefor the title “High Carbohydrate Intake Worse than High Fat for Blood Lipids”.
I think it’s highly likely that LDL-C in elevated levels is only harmful if the particle count/size is out of order. In fact the average LDL-C level of first MI is considerably lower than the averagel LDL-C in the population.
If reduction of LDL-C reduces CV events, why does it only do so if lowered by statins?
Answer: Because it’s not the cholesterol lowering that’s doing the trick, but the other effects of statins.
To illustrate this, the Mediterranean diet has a bigger effect on the disease than statins, without changing the LDL-C.
The problem is, Axel, these experts don’t read anything like enough 🙁
These association studies seem draw lot of attention. Unfortunately their value as evidence is very weak, much weaker than prospective cohort studies that often ridiculated by low-carb tribe. Randomized feeding studies are superior in showing true causality between diet and lipid/sugar values. Luckily we have plenty of them. Clarke BMJ 1997, Mensink AJCN 2003, Imamura Plos One 2016 & one that Erik Andersen points here out to start with. These meta-analyses paint a bit diffferent picture.
But apropos ecological correlation studies, one is just out that shows meat-protein is associated with obesity globally? Should you cover it without covering the context, ie. the results of heaps of randomized and prospective studies?
Thanks Reijo.
You are almost always the voice of reason so I’m finding it hard to believe that you’re suggesting we should just ignore the PURE data because there is contradictory evidence available. In fact, as pointed out in the abstract, this is the first study addressing this question in people living in low and middle income countries.
I’m aware of the problems associated with the methodology. However, a study this large should be able to reveal a pattern if there is one. Of course we need more data to understand what’s going on. For example, we need breakdown of the macronutrients. To what extent are we talking about refined carbohydrates and added sugar? We don’t know that yet. The document Erik Arnesen forwarded also shows that different types of saturated fats affect lipids differently, something that is often forgotten.
I’m not suggesting that the PURE data have finally revealed the truth but let’s not just wipe this under the rug.
Even the meat protein study, if you follow the line of thinking in the other publications by that group, is based on the hypothesis that high-sugar diets delay the digestion and impair the metabolism of protein. You in the press release seems to be suggesting that we should limit protein to better tolerate high-sugar diets. Yet experimental evidence shows that replacing sugar with protein improves the parameters (BMI, liver enzymes) that their hypothesis was based on. I’m not aware of any research on replacing protein with sugar, but I’m not expecting great things. The fact that populations with better access to food increase their intake of animal protein as well as sugar is probably something that limits harm in those populations, compared to all the increase in BMI being associated with a rise in sugar intake, because at least the animal protein is not empty calories, and these populations are transitioning from deficiency diseases to diseases of excess.
“However, a study this large should be able to reveal a pattern if there is one.”
In studies like this: does the word “ecological fallacy” ring a bell?
As Reijo pointed out, both metabolic ward studies and prospective cohort studies paint a very different picture. Consider the PUFA findings: there is no mechanism explaining the higher ApoB levels from increased PUFA consumption and PUFA is clearly superior to MUFA in LDL-C and TG levels. If ecological data contradicts data from metabolic ward studies in risk markers, it should be a no-brainer which to trust.
On Wednesday I sat through another exhausting lunch and learn where a nutritionist told a room full of diabetics that they should be getting 55-60% of their caloric intake from simple carbohydrates. It was all I could do to hold my tongue. Why tell someone who can’t metabolize carbohydrates to make them more than half of their diet. It doesn’t make sense to me. And personal experience while on the South Beach diet taught me that my cholesterol levels were much better than on the ADA recommended diet. I am so happy to finally have a study to vindicate my experience.
“The authors concluded that higher carbohydrate intake has the most adverse impact on lipid profiles and replacing it with saturated fat improved HDL-C and TG and replacing it with mono-unsaturated improved TC/HDL-C and ApoB/ApoA.”
As the “carbs –> SAFA” produced mostly insignificant results (according to trial data, increasing HDL-C seems to mostly much ado about nothing & SAFA tends to impair HDL functionality), detrimental results (increase in LDL-C) and partially … well, results the benefits of which a bit of beneficial to some (decrease in TG), the authors’ conclusion seems at least somewhat erroneous.
I am in 100% Agreement the pyramid is wrong. Ive lost 9 pant sizes sine May 2015, by eliminating starchy sugary carbs. Rarely desire snacks like I used to. Saturated animal based fats keep me sasiated for hours. I don’t eat junk food. Accept McDonalds triple 1/4 Lb. er and I ask for NO KETCHUP & NO BUN. My weight has stabilized right where it should be. Also #keto #LCHF lost all that weight at 63 post menapause without rigorous exercize. Just the normal day to day activities!
Thanks for sharing this study. This data ads weight to the possibility for crafting a simpler and more useful public health message with a focus on refined carbohydrate reduction and greater use of MUFAs.
Shopping, thought I’d buy cream cheese, well, the marketplace has 6 varieties of LOW FAT cream cheese and only one original. This is indicative of the effect that false claims regarding sat fat and heart disease has had, reducing the size of our meat consumption, by raising the prices astronomically on all the healthier choices, meat, cheese, green vegetables forcing most uniformed working class people with children to buy refined carbohydrates, and the diobesity (obesity) in children continues…. Simply by shifting towards increased profits for the medical world with pharmaceuticals with a direct link to all the major gmo grain producers, plus sugary fruit and low fat starches. Take money from those guys and give it to our guys. Just follow the money. The news media helps disseminate these promotional mis-guided pseudo UnFACTS and unfortunately, too many people depend on their TV major network news organizations for factual evidence unbiased reporting, when in fact they are the mouth pieces of their financial sponsors, who surprisingly? they are big pharmaceuticals. With huge government support via lobbyists, and wall street, i.e., global governments.
EAT FAT (animal sources and vegetable) reduce sugar and sugar producing foods unnecessary that really do make the body store fat..
I STRONGLY disagree, Axel with the evidence of MOST experts on Satfat. Where is their endpoint evidence? How about France, Gascony, Switzerland, Spain, Kitava etc. This is nothing more than “received wisdom” which is just plain wrong. How come the RCTs, meta-analyses etc haven’t really shown anything? Didn’t Mozafarian show that satfat slowed progression of CAD in post-MI women? You CANNOT explain Gascony if satfat bad. I put it to Lee Hooper in a meeting and she couldn’t give an answer. Satfat associated with ref.carbs does make you fat etc by an incretin effect, but blame the carbs.
In medicine we are dealing with a huge echo-chamber. It’s got to stop. Yudkin had the answer. His book should be compulsory reading for medical people,
Garry
I agree with you Garry.
There may be instances where it is advisable to lower the amount of saturated fat consumed.
However, the main issue is the source.
Of course, some foods containing saturated fat cannot be considered healthy, but that’s usually not because of the saturated fat per se.
So, in my opinion, the general recommendation to avoid saturated fat is misleading and may increase the risk of unhealthy food chioces.
How does apoE4 influence this thinking? Does the harm of apoE4 increase the more saturated fat one eats? Does LDL-P tell you anything about harm from apoE4? Conversely, is higher saturated fat good for apoE3 because of the many protective functions of apoE3?