For years, physicians have debated the best approach to evaluating stable chest pain.
An ideal diagnostic test should enhance accuracy while minimizing risks to patients, simultaneously improving prognosis and reducing overall health risks.
Now, the SCOT-HEART trial provides definitive long-term evidence that Coronary CT Angiography (CCTA) not only improves diagnosis but also significantly reduces heart attacks and heart-related deaths over time. With its 10-year follow-up published last January in The Lancet, this study challenges traditional approaches and reinforces the role of CCTA in modern cardiology (1).
Here, I shall summarize the latest findings, review previous results from the SCOT-HEART trials, and discuss the clinical implications of these discoveries.

The Challenge of Diagnosing Coronary Artery Disease
Diagnosing coronary artery disease (CAD) can be complex, as symptoms such as chest pain may arise from various conditions, ranging from harmless musculoskeletal pain to life-threatening blockages in the coronary arteries. The challenge in diagnosing CAD is twofold:
- Missing a serious condition: A missed diagnosis can lead to heart attacks or sudden cardiac death. Hence, early and accurate detection is crucial.
- Over-testing: Unnecessary tests and procedures can lead to patient anxiety, increased healthcare costs, and potential complications, without significantly improving outcomes.
Striking the right balance requires careful patient selection and appropriate use of non-invasive tests.
Alternative Methods for Diagnosing Coronary Artery Disease
Before deciding on CCTA or other advanced imaging, physicians often use a range of diagnostic tools, including:
- Electrocardiogram (ECG): Assesses heart rhythm and detects signs of ischemia.
- Exercise Stress Testing: Evaluates the heart’s response to exertion to help detect ischemia (2).
- Stress Echocardiography: Uses ultrasound imaging to assess heart function during stress (3).
- Myocardial Perfusion Imaging (MPI): A nuclear medicine test evaluating blood flow to the heart muscle.
- Cardiac MRI: Provides detailed imaging of heart structure and function, sometimes used for ischemia assessment.
Each of these tests has strengths and limitations, making proper patient selection critical.
Who Should Undergo Coronary Angiography?
Coronary angiography is the gold standard for diagnosing significant CAD but is an invasive procedure with associated risks. It is typically reserved for:
- Patients with high-risk features on non-invasive testing.
- Those with persistent or worsening symptoms despite medical therapy.
- Individuals with a high clinical suspicion of significant coronary stenosis.
- Patients with known CAD being considered for revascularization (stenting or bypass surgery).
The SCOT-HEART trial’s findings suggest that CCTA is a valuable tool for identifying which patients should be referred for coronary angiography, improving patient selection and reducing unnecessary invasive procedures.
Background: What Is the SCOT-HEART Trial:?
The Scottish Computed Tomography of the Heart (SCOT-HEART) trial was designed to determine whether CCTA improves the diagnosis and management of CAD compared to standard care alone. Conducted across multiple cardiology centers in Scotland, it enrolled over 4,000 patients with suspected stable angina (4).
Key Goals of the SCOT-HEART Trial:
- Determine if CCTA improves diagnostic accuracy for CAD.
- Assess whether CCTA reduces major cardiovascular events, including heart attacks and deaths.
- Evaluate the impact of CCTA on medical therapy and invasive procedures.
The first results, published in 2015, showed that CCTA led to more accurate diagnoses and changes in treatment decisions.
Later follow-up results (5-year and 10-year data) confirmed the long-term benefits of using CCTA in stable chest pain evaluation (5, 1).
The 10-Year Results: What Did the Study Find?
The recently published 10-year results of the SCOT-HEART trial reinforce the value of CCTA in long-term cardiovascular prevention. Here are the key takeaways:
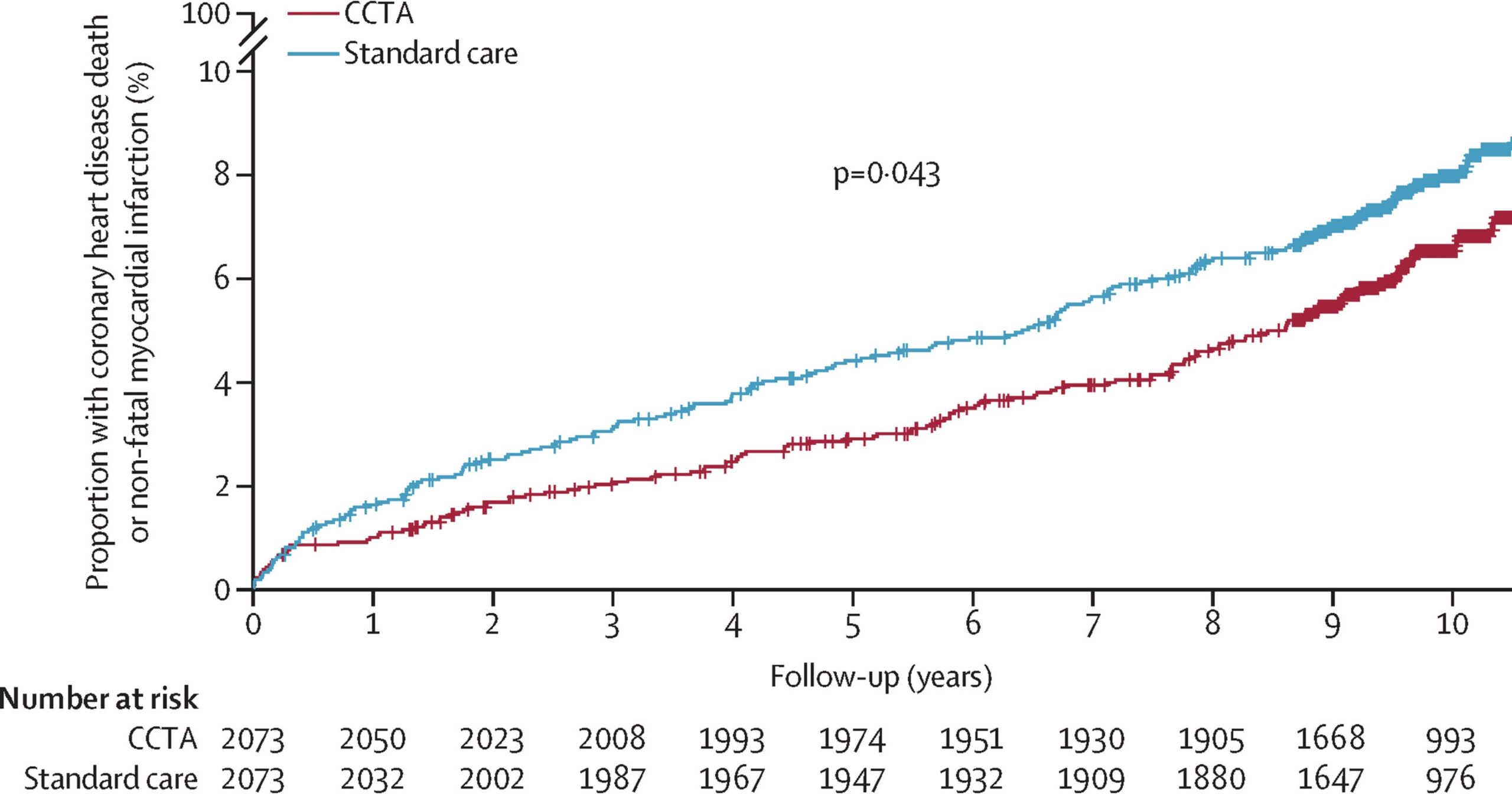
- Lower risk of heart attacks: The CCTA group had a 21% lower risk of coronary heart disease death or non-fatal heart attack compared to the standard care group.
- Improved use of preventive therapy: More patients in the CCTA group were prescribed statins and aspirin, helping lower their risk over time.
- No increase in unnecessary procedures: The number of people undergoing invasive procedures (such as stents or bypass surgery) was similar between both groups, meaning CCTA did not lead to excessive interventions.
The absolute risk reduction (ARR) for the composite endpoint of coronary heart disease death or nonfatal myocardial infarction was 1.6% over a median follow-up of 4.8 years with a sustained benefit over a median follow-up of 10 years. This equates with a number needed to treat (NNT) of 63 patients receiving CCTA to prevent one event.
This means that for every 1,000 patients evaluated with CCTA, approximately 16 future heart attacks or cardiac deaths are prevented—without increasing unnecessary procedures.
How Do These Results Compare to Previous SCOT-HEART Findings?
The SCOT-HEART findings have been consistent over time:
- 2015 Results: CCTA improved the accuracy of CAD diagnosis and helped doctors make better treatment decisions.
- 5-Year Results (2018): Showed a 41% reduction in heart attacks in the CCTA group compared to standard care.
- 10-Year Results (2024): Show sustained benefits in reducing heart attacks and deaths without increasing the need for invasive procedures.
These findings reinforce that CCTA should be an essential tool in evaluating stable chest pain and preventing heart disease progression.
Clinical Implications: How Should This Change Practice?
The SCOT-HEART trial’s findings suggest that CCTA should become a first-line test for stable chest pain, as recommended by both European and American guidelines (6, 7)
Here’s why:
- More Accurate Diagnoses: CCTA provides detailed images of both soft and calcified plaques, improving the identification of coronary artery disease.
- Better Preventive Care: Early detection through CCTA allows doctors to prescribe lifestyle changes and medications (statins, aspirin) sooner, reducing long-term risk.
- Fewer Unnecessary Procedures: Unlike traditional angiography, CCTA prevents unnecessary invasive procedures while ensuring that those who truly need them receive appropriate care.
Are There Cost Considerations?
One potential concern is the cost-effectiveness of routine CCTA use.
The SCOT-HEART results suggest that while CCTA has upfront costs, it may reduce long-term healthcare costs by preventing expensive hospitalizations, heart attacks, and interventions.
Further economic analyses will be important in determining how widely CCTA should be used in different healthcare systems.
Final Thoughts: Why SCOT-HEART Matters?
The SCOT-HEART trial is a landmark study with game-changing implications.
The findings make a compelling case for CCTA as the preferred first-line test for stable chest pain.
Physicians should embrace this technology not just for its diagnostic accuracy, but for its ability to prevent cardiac events.
This article was written with the assistance of ChatGPT, an AI language model developed by OpenAI, to help refine and structure the content.

Thanks for the discussion. Unfortunately, CCTA suffers from a major drawback, blooming artifact, which can lead to over-interpretation. I had a CCTA report which was very worrisome. I had the data run through the CLEERLY software, which gave a much better picture, reducing degree of stenosis, but more importantly quantifying unstable versus stable plaque. I will send you the the two reports so you can see the significant difference. I think the CLEERLY software is not well know in the cardiology community but offers very significant benefit.
Thanks Bob
Very interesting. I have no experiance with CLEERLY.
I agree, blooming effect form calcium or stents is a classic issue, but its getting better all the time.
Impressive results, indeed. CCTA not to be only a diagnostic, but also preventive procedure. I was so impressed that I have taken a look on the original article published in Lancet.
Following that I would like to reflect on the conclusion in your summary: “The key takeaway from the SCOT-HEART trial is clear: CCTA leads to a 21% reduction in heart attacks and coronary deaths. This means that for every 1,000 patients evaluated with CCTA, approximately 20 future heart attacks or cardiac deaths are prevented—without increasing unnecessary procedures.” I think there is a typo… It should be probably: “The key takeaway from the SCOT-HEART trial is clear: CCTA leads to a 21% reduction in heart attacks and coronary deaths. This means that for every 100 patients evaluated with CCTA, approximately 20 future heart attacks or cardiac deaths are prevented—without increasing unnecessary procedures?” Thank you for your feedback.
Hi Maja.
I appreciate your attention to detail regarding the key takeaway from the SCOT-HEART trial.
In order to calculate the NNT (number need to treat) you need to look at absolute (not relative) risk reduction.
I did a recalculation:
Absolute risk reduction (ARR) is essential for calculating the number needed to treat (NNT). In the SCOT-HEART trial, the ARR for the composite endpoint of coronary heart disease death or nonfatal myocardial infarction was 1.6% over a median follow-up of 4.8 years. This means that for every 1,000 patients evaluated with coronary computed tomography angiography (CCTA), approximately 16 future heart attacks or cardiac deaths are prevented—without increasing unnecessary procedures.
To calculate the NNT, you can use the formula: NNT = 1 / ARR. Applying this to the SCOT-HEART trial data: NNT = 1 / 0.016 = 62.5, which rounds up to 63. Therefore, 63 patients would need to undergo CCTA to prevent one additional event of heart attack or cardiac death.
This NNT compares favorably to many established cardiovascular therapies, highlighting the potential benefit of CCTA in this context.