Estimated reading time: 11 minutes
Menopausal hormone therapy is an effective treatment for hot flashes associated with menopause. It may also help prevent bone loss (osteoporosis) and reduce the risk of bone fractures in postmenopausal women.
However, menopausal hormone therapy may also be associated with risks for the patient. The risks depend on the individual treated, the type of hormone therapy, and the dose and length of treatment (1).

Estrogen is the hormone that provides the most menopausal symptom relief. Progestogen is commonly added to protect women against uterine cancer from estrogen alone.
Systemic estrogen (available as pill, skin patch, gel, cream or spray) is the most effective treatment for the relief of hot flashes.
Vaginal preparations of estrogen are often effective for vaginal and urinary symptoms, but they do not reduce the severity of hot flashes.
In the United States, vaginal estrogen is available in a handful of low-dose preparations, such as estrogen creams (Estrace Vaginal Cream and Premarin Vaginal Cream), a tablet (Vagifem), and an estrogen-infused vaginal ring (Estring).
Menopause, Perimenopause, and Postmenopause
Menopause occurs when the ovaries naturally begin to decrease their production of estrogen and progesterone. It is defined as the time when there have been no menstrual periods for 12 consecutive months, and no other biological or physiological cause can be identified (2).
Menopause usually occurs between 45 and 55 years of age. The average age in the United States is 51.5 years (3).
The menopause transition begins about six years before the natural menopause. This period is called perimenopause.
During perimenopause, the levels of hormones produced by the ovaries fluctuate, resulting in irregular menstrual patterns.
The average length of perimenopause is four years. However, in some women, it may last only a few months or continue for ten years. Menopausal symptoms usually begin during perimenopause.
The term ‘postmenopause’ describes all the years beyond menopause.
Menopausal Symptoms
Hot flashes are the most common symptom associated with menopause (4).
Hot flashes are a sudden sensation of heat in the chest, face, and head that rapidly become generalized. Up to 80% of women going through menopause experience such symptoms (5).
The sensation of heat usually lasts for a few minutes and is often associated with palpitations and profuse sweating (6). Sometimes hot flashes are followed by chills, shivering, and a sensation of anxiety.
Some women only experience occasional hot flashes while some may have repeated episodes many times each day.
Hot flashes can severely impact daily life and functioning, particularly when they disrupt sleep, sometimes leading to fatigue and irritability during the day.
Other menopausal symptoms include vaginal dryness, sleep disturbances, breast pain, migraines, problems with memory loss, difficulty concentrating, and new-onset depression (7).
Menopausal Hormone Therapy
Menopausal hormone therapy is a term that is used to describe estrogen treatment for women suffering from menopausal symptoms.
The term applies to both unopposed estrogen for women who have undergone hysterectomy (removal of the uterus) and combined estrogen-progestin therapy for women with an intact uterus.
The primary goal of menopausal hormone therapy is to relieve menopausal symptoms, most importantly, hot flashes.
Other symptoms, such as vaginal dryness, dyspareunia, mood lability, and sleep disturbances, are often improved as well.
The Early History
In 1942, the FDA approved Premarin, for treatment of hot flashes. Premarin is a mixture of estrogen hormones isolated from pregnant mares (8).
The drug was highly effective and provided great relief for hot flashes, igniting hope for millions of women that their quality of life might be dramatically improved during the menopausal transition.
In the 1960s and 1970s, the list of reasons why women should take estrogens rapidly grew more substantial. In a few years, pharmaceutical companies successfully and cannily managed to turn these drugs into a billion-dollar panacea for aging women(9).
Interestingly, all this happened despite warning flags being raised because scientific data brought forward in the 1970s suggested that hormone therapy might be linked to cancer of the uterus.
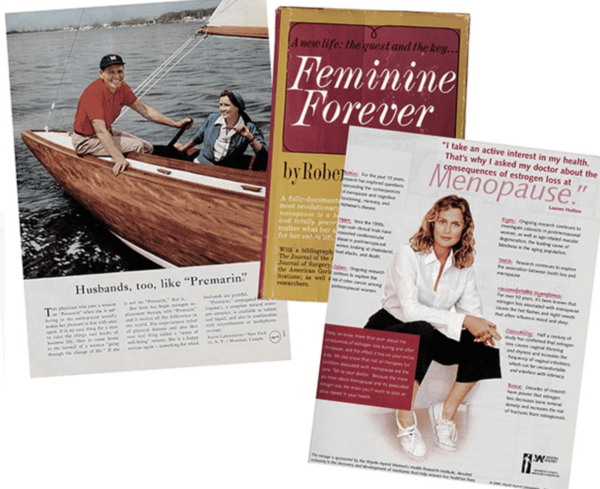
In 1966, the book “Feminine Forever” became a best seller claiming that “menopause is completely preventable.”The book’s author, Robert A. Wilson, wrote that because estrogen levels drop, postmenopausal women who didn’t receive treatment were no longer genuinely female. Wilson traveled the country, lecturing on this topic and promising that with the help of estrogen therapy, “Every woman alive today have the option to remain feminine forever (8).”
Eleven years later, in 1977, Barbara Seaman’s book “Women and the Crisis in Sex Hormones” alerted women to evidence that taking hormones could cause breast cancer, strokes, and blood clots. The book became a best seller and played an essential role in educating a generation of women about the health risks of hormones.
However, encouraged by research suggesting that hormone treatment might be helpful for the prevention of heart disease, many medical professionals continued to recommend menopausal hormone treatment.
In 1995, approximately 38% of postmenopausal women in the United States used hormone replacement therapy, mostly to treat symptoms of menopause and prevent chronic conditions such as cardiovascular disease and osteoporosis. (10).
It was not until the publication of the Women’s Health Initiative (WHI) Trial in 2002 that things started to change.
Hormone Replacement Therapy and Heart Disease
It is a longheld belief that estrogen may protect against cardiovascular disease. Before the late 1990s, hormone replacement therapy was recommended for both primary and secondary prevention of cardiovascular disease (11)
Coronary heart disease (CHD) is uncommon in women before 50 years of age. Postmenopausal women demonstrate an increased risk of CHD compared to premenopausal women of the same age. Furthermore, there is an increased risk of CHD after premature menopause. All these facts initially lend support to the estrogen-CHD hypothesis suggesting that declining estrogen levels may cause the increased risk of CHD following menopause (12).
Observational studies have almost universally reported a lower risk of CHD in postmenopausal women receiving hormone replacement therapy as compared with those women who are not (13).
In 1998 the Heart and Estrogen/ Progestin Replacement Study (HERS) was the first trial to cast severe doubts on the proposed benefits of menopausal hormone treatment. The study reported an increase in cardiovascular events among women with a history of cardiovascular disease treated with conjugated equine estrogen and medroxyprogesterone acetate (14).
Subsequently, hormone therapy was considered inappropriate for secondary prevention but still retained a role of primary prevention of cardiovascular disease. In other words, it was thought that the HERS results did not apply to healthy women.
The Women’s Health Initiative (WHI), was the first randomized clinical trial to assess hormone therapy for healthy women.
The study results, presented in 2002, reported an increased risk of breast cancer and cardiovascular events in women without pre-existing cardiovascular disease randomly assigned to receive conjugated equine estrogen and medroxyprogesterone acetate (15).
For every 10,000 person-years of combination menopausal hormone therapy use, there were seven more heart attacks, eight more strokes, eight more blood clots on the lungs, and eight more invasive breast cancers.
It was concluded that the overall health risks exceeded benefits from the use of combined estrogen plus progestin among healthy postmenopausal women.
The study primarily demonstrated adverse effects of menopausal hormone therapy in older postmenopausal women (over age 60 or more than ten years since menopause)(16).
In the ensuing years, the amount of menopausal hormone replacement being prescribed fell by half (17).
Following the publication of the WHI trial, guidelines were revised to recommend against the routine use of hormone therapy for reasons other than the treatment of menopausal symptoms, and that treatment should continue for the shortest duration possible.
Menopausal Hormone Therapy and Osteoporosis
Menopause predisposes women to osteoporosis due to declining estrogen levels.
Osteoporosis results in a decrease in bone mineral density and an increased risk of bone fractures. Osteoporotic bone fractures are considered one of the largest public health priorities by the World Health Organization (WHO)(18).
Randomized controlled trials and observational studies have shown that hormone replacement therapy reduces postmenopausal osteoporotic fractures of the hip, spine, and all non-spine fractures in women with and without osteoporosis (19,20).
In 2016, The International Menopause Society (IMS), stated that in the age group 50–60 years or within ten years after menopause, the benefits of hormone therapy are most likely to outweigh any risk and can be considered as first-line therapy for fracture prevention (21).
Conversely, the American College of Physicians (ACP) recommended against menopausal hormone therapy in their clinical practice guideline for the treatment of osteoporosis in women, stating that high-quality evidence from the WHI trial showed that such treatment was associated with increased risk for cardiovascular events and invasive breast cancer (22). In their view, treatment with bisphosphonates (alendronate, risedronate, zoledronic acid), or denosumab is to be preferred.
The Benefits of Menopausal Hormone Therapy
Most menopausal symptoms are triggered by a marked decrease in ovarian estrogen production invariably associated with menopause.
Menopausal hormone therapy (estrogen alone or combined with progestin) is the most effective treatment available for relief of menopausal symptoms such as hot flashes, vaginal dryness, and dyspareunia (difficult or painful sexual intercourse)(23). The main goal of menopausal hormone therapy is to relieve such symptoms.
Hot flashes are the most common indication for hormone therapy. Although alternative treatments are available, none are as effective as estrogen.
Women who are primarily being treated for vaginal dryness or vulvovaginal atrophy should be treated with low-dose vaginal estrogen rather than systemic estrogen.
Menopausal hormone therapy is effective for women who suffer from depression or mood lability. Sometimes they are used in combination with other antidepressant drugs such as selective serotonin reuptake inhibitors (SSRI).
There is some evidence that estrogen me preserve cognitive function and prevent dementia. However, clinical trial evidence is currently not strong enough to recommend such treatment. Furthermore, the risks associated with hormone treatment seem to increase with higher age.
A recent meta-analysis suggests that menopausal hormone therapy does not affect the risk of death from all causes, cardiac death, and death from stroke or cancer (15).
Based on data from the WHI trial, menopausal hormone therapy should not be used to prevent cardiovascular disease (14).
Menopausal hormone therapy is generally considered safe in women within ten years of menopause or younger than age 60 years unless contraindications are present.
Combined hormone therapy (estrogen-progestin) appears to reduce the risk of type 2 diabetes (24). However, current data is insufficient to recommend hormone therapy for the prevention of diabetes in postmenopausal women.
The Risks of Menopausal Hormone Therapy
The WHI trial demonstrated adverse effects of hormone replacement therapy in menopausal women over 60 years of age or more than ten years since menopause.
Evidence suggests that the risks of hormone therapy in younger postmenopausal women are considerably lower than in older women (16).
In the WHI trial, the risk of invasive breast cancer was significantly increased with combined hormone therapy.
Studies have shown that treatment with estrogen alone is associated with an increased risk of cancer of the uterus (25). This risk may be largely abolished by using combined estrogen-progestin treatment.
A recent epidemiological study of the risks of systemic hormone therapy shows that women who started around the time of menopause were at greater risk of invasive breast cancer than apparently similar never users (26).
Excess risks were greater among current than past users, but some risk persisted for more than a decade after hormone therapy was stopped.
There was little excess risk after of hormone therapy for less than 1 year, but there were definite excess risks associated with just 1–4 years of use, and progressively greater risks with longer use.
The risk was greater for estrogen-progestagen than for oestrogen-only preparations, particularly if progestagen use was daily rather than intermittent.
The study did not address vaginal preparations of estrogen. To date, there is no evidence that vaginal estrogen increases the risk of cancer.
Women with a history of breast cancer, coronary heart disease, stroke, or a previous venous thromboembolic event should not receive menopausal hormone treatment. This is true also for women with active liver disease.
Based on data from the WHI trial, women with gallbladder disease should not receive hormone therapy.
The Duration of Hormone Replacement Therapy
In most cases, short-term hormone treatment is considered the most sensible option. Short-term therapy is considered to be less than five years (or not beyond age 60 years) (27).
However, in about one-quarter of cases, hot flashes persist after discontinuation of hormonal therapy (28).
Persistent hot flashes after stopping hormone treatment can severely impact quality of life. Hence, extended use of hormone therapy may be warranted when the clinician and the patient agree that the benefits outweigh the risk.
The Bottom Line
Many forms of estrogen are available; oral, transdermal, topical gels, vaginal creams, tablets, and rings.
It is essential to use an individualized approach when deciding whether a woman should receive hormone therapy or not. Before treatment is initiated, the woman’s risk of cardiovascular disease and breast cancer should be assessed.
The main argument for treatment is the management of menopausal symptoms such as hot flashes. Menopausal hormone therapy should not be used for the prevention of heart disease, osteoporosis, or dementia.
Treatment is not recommended for women older than 60 years, or more than ten years from menopause.
The risk of breast cancer appears to be significantly increased with combined systemic hormone therapy.
However, there is no evidence that vaginal estrogen increases the risk of cancer.
If a decision is made to give menopausal hormone treatment, the type of drug and the route of administration have to be determined.
Women with an intact uterus should not be given estrogen alone but a combination of estrogen and progestin.
Women who are primarily being treated for vaginal symptoms should be treated with low-dose vaginal rather than systemic estrogen.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

transdermal estradiol does not seem to be associated with increased risk of stroke or VTE. Transdermal administration avoids first pass hepatic metabolism with less hepatic induced coagulation and inflammatory effects.
Transdermal hormone therapy and the risk of stroke and venous thrombosis.
Speroff L Climacteric. 2010 Oct;13(5):429-32. doi: 10.3109/13697137.2010.507111.
PMID:20670199
Hormone replacement therapy and the risk of venous thromboembolism: a population-based study.
Renoux C, Dell’Aniello S, Suissa S.
J Thromb Haemost. 2010 May;8(5):979-86. doi: 10.1111/j.1538-7836.2010.03839.x. Epub 2010 Mar 4.
PMID:20230416
Maturitas. 2015 Nov;82(3):304-7. doi: 10.1016/j.maturitas.2015.06.040. Epub 2015 Jul 26.
Hormone therapy and risk of venous thromboembolism among postmenopausal women.
Canonico M1.
Likewise no increased breast cancer risk with TD E2 with progesterone (Fournier, Unequal Risks….Breast Ca Res Treat. 2008, 101(1):103
WHI looked at Equine estrogen source, not bio-identical HRT.
So risk benefit balance with TD E2 + progesterone is different when compared to equine estrogen source.