Estimated reading time: 12 minutes
Most women will experience hot flashes when going through the menopause.
In the USA, the term hot flashes is used to describe this phenomenon whereas in the UK the term hot flushes is used. Both mean the same thing.
Hot flashes are also known as vasomotor symptoms. The term ‘vasomotor’ refers to the vasomotor center in the brain which plays an important role in regulating peripheral blood flow and blood pressure.

Menopausal hot flashes may be described as a sudden feeling of warmth, that seems to come from nowhere and spreads throughout the body, usually most intense over the face, neck, and chest. Sometimes the hot flashes are accompanied by sweating, palpitations, and reddening of the skin.
Some women only have mild symptoms with occasional hot flashes that don’t really affect their quality of life, while others can have many a day, and find them very uncomfortable, disruptive and sometimes embarrassing.
Hot flashes have been consistently shown to be associated with discomfort, sleep disturbances, fatigue, and decreased quality of life.
Pregnancy and childbirth are pretty rotten jokes to play on the female, but I cannot help suspecting that the menopause may be nature’s last — and most outrageous — grand belly laugh.
― Elizabeth Oakleigh-Walker Buchan, “Rite of Passage,” 1993
1. What Is Menopause?
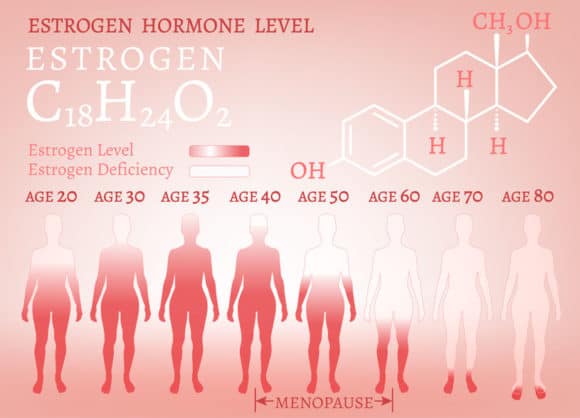
The natural menopause is the time in a woman’s life when she stops having periods. It occurs when the ovaries naturally begin to decrease their production of the sex hormones estrogen and progesterone. Menopause marks the end of fertility and childbearing years.
Induced menopause occurs if the ovaries are surgically removed or damaged, for example by radiation or drugs.
Menopause is defined as the time when there have been no menstrual periods for 12 consecutive months, and no other biological or physiological cause can be identified (1).
Periods usually start to become less frequent over a few months or years before they stop altogether.
The menopause is a natural part of aging and usually occurs between 45 and 55 years of age. The average age of menopause in the United States is 51.5 years (range, 45-59 y) (2).
Premature menopause (before 40 years of age) occurs in approximately 1 in 100 women. Women who smoke are likely to go into menopause earlier than those who don’t smoke (3)
The term ‘postmenopause’ describes all the years beyond menopause.
2. What Is Perimenopause (Menopause Transition)?
The changes of the menopause transition begin about six years before the natural menopause. This period is called perimenopause.
During perimenopause, the levels of hormones produced by the ovaries fluctuate, resulting in irregular menstrual patterns. Usually, there is an irregularity in the length of the period, the time between periods, and the level of flow.
The average length of perimenopause is four years, but for some women, it may last only a few months or continue for ten years. Perimenopause ends when a woman has gone 12 months without having her period.
Menopausal symptoms usually begin during perimenopause.
3. What Are Menopausal Symptoms?
The most common symptom during the menopausal transition and menopause is hot flashes.
Women may experience a number of other symptoms, including vaginal dryness, sleep disturbances, breast pain, migraines, problems with memory loss and difficulty concentrating, and new-onset depression (4).
Changes in lipids and bone loss often begin to occur during premenopause.
4. What Are Menopausal Hot Flashes?
Hot flashes, also known as vasomotor symptoms, are often described as a sudden sensation of heat in the chest, face, and head that rapidly become generalized.
The sensation of heat usually lasts for two to four minutes and is often associated with profuse sweating and sometimes palpitations (5).
Sometimes hot flashes are followed by chills, shivering, and a sensation of anxiety.
Some women only experience occasional hot flashes while some may have repeated episodes, sometimes every hour during day and night.
Hot flashes may mark adverse underlying vascular changes among midlife women (6). They may also be a marker for risk of bone loss (7).
5. How Common Are Hot Flashes?
Up to 80% of women going through menopause experience hot flashes (8).
However, only approximately 20 to 30 percent of women seek medical attention for treatment (5).
Women with perimenopause shorter than six months (estimated at 10% of women) have lower rates of hot flashes (9).
6. When Do Hot Flashes Begin and How long Do They Last?
Although the average age of menopause is approximately 51 years, hot flashes can start well before the final menstrual period and last for several years after the onset of menopause.
Recent studies have demonstrated that the average duration of menopausal symptoms such as hot flashes is approximately 7 to 9 years (10).
Early evidence suggested that the prevalence of hot flushes accelerates during perimenopause, peaks at about the time of the last menstrual period and declines rapidly after that (11).
However, even though the frequency and severity of hot flashes decrease with age for most women, some continue to report persistent symptoms even into their seventh and eighth decades of life.
A recently published study from the Mayo Clinic showed that flashes may still be disruptive in women over a decade past the natural age of menopause (12).
One study showed that African American women had a longer total duration of hot flashes, whereas Chinese and Japanese women had shorter total duration. (13).
7. What Causes Menopausal Hot Flashes?
Menopausal hot flashes are mediated by thermoregulatory dysfunction at the level of the hypothalamus (14). The dysfunction appears to be initiated by low estrogen levels, the hallmark of the menopausal transition. Elevation of luteinizing hormone (LH) co-occurs.
The feeling of heat is caused by peripheral vasodilatation (the widening of blood vessels). Hence, the term ‘vasomotor symptoms’ is often used to describe hot flashes.
When peripheral blood vessels dilate, skin blood flow is increased causing a feeling of warmth.
Perspiration may lead to rapid heat loss. Shivering may then occur to restore the core temperature to normal (5).
8. What Factors Increase the Risk of Hot Flashes?
Several characteristics and health behaviors have been reported to be significantly associated with an increased risk of hot flashes, including cigarette smoking, obesity, and lower levels of education (15).
Obese women have a higher risk of hot flashes (16).
One study showed that among women who were overweight or obese and had bothersome hot flushes, an intensive behavioral weight loss intervention resulted in improvement in flushing (17).
Current smoking may predispose a woman to more severe or frequent hot flashes (18).
Socioeconomic factors and low levels of education are associated with an increased risk of hot flashes (19).
Furthermore, African American women report more frequent hot flashes than Caucasian women (19).
9. Can Hot Flashes Cause Sleep Disturbances?
Sleep disturbances are common during the menopausal transition.
An essential feature of hot flashes is that they are more common at night than during the day and are associated with arousal from sleep. Hence, hot flashes that occur at night (night sweats), may be the underlying cause of disrupted sleep.
One study showed that hot flashes accounted for a significant proportion of time awake during the night in perimenopausal women (20).
However, there are many other possible causes of disrupted sleep in this population. Examples are obstructive sleep apnea (OSA), anxiety, and depression.
10. What Nonmedical Treatments May Be Used to Treat Hot Flashes?
There is considerable interest in the development of effective nonmedical interventions to help women manage hot flashes
Simple measures such as lowering room temperature, using fans, dressing in layers of clothing that can be easily shed, and avoiding triggers (such as spicy foods, too much alcohol, and stressful situations), can help reduce the number of hot flashes (5).
Growing evidence from recent randomized controlled trials suggests that cognitive-behavior therapy (CBT) can effectively reduce the impact of hot flushes (21).
CBT seems to work mainly by changing symptom perception and cognitive appraisal.
Hypnosis may be beneficial for hot flashes (22), but there is limited data available on its efficacy.
Results of one placebo double blind-controlled trial suggest that vitamin E may reduce the frequency and severity of hot flashes (23).
Herbal remedies such as black cohos are used by many postmenopausal women for hot flashes. However, clinical trials have shown that it is not more effective than placebo (24).
There have been concerns that black cohosh could stimulate breast tissue like estrogen, increasing the risk of recurrence in women who have had breast cancer. However, so far, there is no evidence that it is harmful, even in women with breast cancer.
There are a variety of plant-based treatments available for the treatment of hot flashes. Isoflavones and phytoestrogens, found in many plants, fruits, and vegetables, are commonly used.
Phytoestrogens also called ‘dietary estrogens,’ are a diverse group of naturally occurring nonsteroidal plant compounds that have structural similarity with estradiol. They are found in many foods, including soybeans, chickpeas, lentils, flaxseed, lentils, grains, fruits, vegetables, and red clover.
Isoflavone supplements, a type of phytoestrogen, can be purchased in health food stores.
A systematic review of plant-based therapies published 2016 showed that phytoestrogen supplementations were associated with modest reductions in the frequency of hot flashes and vaginal dryness but no significant reduction in night sweats (25)
However, it is still considered uncertain whether phytoestrogens help to reduce hot flashes as most studies have not reported benefit. Furthermore, some phytoestrogens might act like estrogen in some tissues of the body.
Many experts suggest that women who have a history of breast cancer should avoid phytoestrogens.
11. What Is the Role of Hormonal Therapy?
Hormone replacement therapy is effective for the treatment of hot flashes.
Hormone therapy may also help prevent bone loss and reduce the risk of bone fractures in postmenopausal women.
However, there are also risks associated with menopausal hormone therapy. These risks depend on the individual treated, the type of hormone therapy administered, and the dose and length of treatment.
Estrogen is the hormone that provides the most menopausal symptom relief. Progestogen is added to protect women against uterine (endometrial) cancer from estrogen alone.
The general rule is that women with an intact uterus are given both estrogen and a progestin, while those who have undergone hysterectomy may be given estrogen only.
Systemic estrogen (available as pill, skin patch, gel, cream or spray) is the most effective treatment for the relief of hot flashes.
Vaginal preparations of estrogen (available as a cream, tablet or rings) can be effective for vaginal and urinary symptoms but have not been shown to reduce the severity of hot flashes (26).
A combination drug of bazedoxifene with conjugated estrogens (Duavee) has been approved for treating menopausal symptoms. In theory, the risk of uterus and breast cancer might be less with this combination than with estrogen replacement therapy (27).
12. What Are the Risks Associated with Hormonal Therapy?
It is a longheld belief that estrogen may protect against cardiovascular disease. Before the late 1990s, hormone therapy (estrogen with or without progestin) was recommended for both primary and secondary prevention of cardiovascular disease (28).
In 1998 the Heart and Estrogen/ Progestin Replacement Study (HERS) reported an increase in cardiovascular events among women with a history of cardiovascular disease treated with conjugated equine estrogen and medroxyprogesterone acetate (29).
Subsequently, hormone therapy was considered inappropriate for secondary prevention but still retained a role of primary prevention of cardiovascular disease.
In 2002, the Women’s Health Initiative (WHI) investigators reported an increase in the composite outcome, including breast cancer and cardiovascular events, in women without pre-existing cardiovascular disease randomly assigned to receive conjugated equine estrogen and medroxyprogesterone acetate (30).
Following the publication of the WHI trial, guidelines were revised to recommend against the routine use of hormone therapy for reasons other than treatment of menopausal symptoms, and that treatment should continue for the shortest duration possible.
Today, hormone replacement therapy is believed to be associated with an increased risk of breast cancer, uterine (endometrial) cancer, stroke and blood clots in the veins. These risks are higher in women over age 60.
Hence, in women with a history of breast cancer, coronary heart disease, a previous venous thrombotic event (blood clot in legs or lungs) or stroke, or those at moderate or high risk for these complications, other therapies should be considered first.
A recent meta-analysis suggests that menopausal hormone therapy does not affect the risk of death from all causes, cardiac death, and death from stroke or cancer (31).
13. For How Long Should Menopausal Hormone Therapy Continue?
In most cases, short-term hormone therapy is considered the most sensible option.
Short-term therapy is considered to be less than five years (or not beyond age 60 years) (32).
However, sometimes hot flashes persist after discontinuation of hormonal therapy. In these cases, non-hormonal therapies (see no. 15 below) may be tried.
For women who experience recurrent, bothersome hot flashes after stopping estrogen, and do not get adequate relief with nonhormonal therapies, extended use of hormone therapy may be considered (33).
14. How Difficult Is It to Stop Menopausal Hormone Therapy?
Most women have no trouble stopping menopausal hormone therapy. Studies show that approximately 75% of women who try to stop can do so without significant difficulty (34).
Approximately one-quarter of women who try to stop report that they are unable to discontinue postmenopausal hormone therapy, mainly owing to the development of hot flashes (35).
Some clinicians recommend slowly tapering hormone therapy to avoid withdrawal symptoms. One study suggests that tapering may lessen recurrence of menopausal symptoms after discontinuation (36)
As persistent hot flashes can severely impact quality of life, extended use of hormone therapy may be warranted when the clinician and the patient agree that the benefits outweigh the risk.
15. Can Nonhormonal Drug Therapy Be Used to Treat Hot Flashes?
Hormone therapy is the most effective therapy for hot flashes. However, non-hormonal drugs are available for the treatment of the condition
Some women are not appropriate candidates for hormone therapy, such as those that have been recently treated for breast cancer.
Non-hormonal therapy may also be tested in women who experience recurrent hot flashes after stopping hormone therapy.
The agents most commonly used include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), antiepileptics, and centrally acting drugs.
Paroxetine (Brisdelle, Paxil), an SSRI that is also used to treat anxiety and depression, is the only nonhormonal medication approved by the Food and Drug Administration for managing hot flashes. However, other related drugs, including SSRIs like fluoxetine (Prozac) as well as norepinephrine reuptake inhibitors like venlafaxine (Effexor), have also shown to be effective.
Gabapentin (Neurontin), a drug also used to treat seizures an nerve pain, may also help against hot flashes.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.

Great article Dr. Sigurdsson! Hot flashes along with several diseases affect women, and no specific remedy exists for them. Many people have found alternative sources of relief, in the form of yoga and tai chi, which have proven to be helpful in alleviating other menopausal symptoms as well.
Hi Evelyn
Thanks for the comment and the kind words.
I have been normal weight (130 lbs at 5′ 5″) for all my adult life, not a smoker and a Dr. of Chiropractic (so not overweight, smoker or under-educated). I had onset of severe hot flashes at the time my periods stopped. They lasted for 9 years. I began taking phytoestrogens when I realized I wasn’t sleeping well and it was affecting my mood. The phytoestrogen combination was (black cohosh, motherwort, chaste tree, sage, licorice extract (low glycyrrhizic) and grape seed extract. This formula reduced the severity of the hot flashes by about 50%. Enough to greatly improve my sleep and my mood.