Estimated reading time: 21 minutes
Dementia is a collective term for a decline in mental ability affecting memory, thinking, behavior, and emotion severely enough to interfere with daily life.
Dementia represents a cluster of symptoms and should not, as such be, considered a disease.

One of the main challenges facing health professionals diagnosing and treating patients with dementia is to define the underlying cause or disease responsible for the patient’s symptoms. In fact, more than one hundred conditions may cause dementia. Alzheimer’s disease is the most common cause accounting for 60-70% of all cases.
Dementia ranges in severity. The mildest stage may be recognized by slight changes in thinking, remembering, and reasoning. In contrast, in the most severe stage, the patient must depend on others’ help for basic activities of living.
Although dementia becomes more common as people age, it should not be considered a normal part of aging. Many people live into their 90s and beyond without any signs of dementia (1).
Due to the aging of the population, the burden of dementia is increasing worldwide.
1. How Common Is Dementia?
Today, more people than before live longer and healthier lives. Hence, the world population has a higher proportion of older people. The fastest growth in the elderly population is taking place in China, India, and the southwestern part of Asia (2).
Worldwide, around 50 million people have dementia. Every year, there are nearly 10 million new cases.
The estimated proportion of the general population aged 60 and over with dementia is between 5-8% (2).
The total number of people with dementia is estimated to reach 82 million in 2030 and 152 million in 2050. Much of this increase is attributable to the increasing numbers of people with dementia living in low- and middle-income countries. Currently, 58% of people with dementia live in these countries. By 2050 this number will have risen to 68%.
Worldwide, around 50 million people have dementia. This number is estimated to reach 82 million in 2030 and 152 million in 2050. Much of this increase is attributable to the increasing numbers of people with dementia living in low- and middle-income countries.
2. What Are the Most Common Dementia Symptoms?
Dementia affects people differently, causing a considerable variation in symptoms between individuals.
Because of the gradual onset of symptoms, the early stage of dementia is often overlooked. Declining memory, especially short-term memory, is the most common early symptom. Other common symptoms include difficulties completing familiar tasks, losing track of time, and becoming lost in familiar places.
Interestingly, most patients with dementia do not by themselves complain of memory loss. It is often a spouse or another close relative who raises a concern (3).
During the next stage, the middle stage, forgetfulness becomes more pronounced. The patient may not remember recent events, and finding his way at home can become more difficult. A person may put things in unusual places, such as glasses in the fridge or a wristwatch in the sugar bowl. There may also be difficulties with communication. Wandering and repeated questioning becomes more prevalent. At this stage, the patient may need help with personal care.
Often there are difficulties with language, and finding the right words may become difficult.
During the late stage of dementia, memory loss usually worsens further. The patient may become unaware of time and place and can have difficulties recognizing relatives and friends. Behavior changes, including aggression, often become more pronounced. The patient may become anxious, suspicious, irritable, and agitated. Some patients may even become depressed or apathetic.
Sometimes passiveness is pronounced. The patient may sit in front of the television for hours, sleep more than usual, or appear to lose interest in hobbies.
3. What Are the Most Common Types of Dementia?
There are many different types of dementia. Alzheimer’s disease is the most common form of dementia and may contribute to 60–70% of cases.
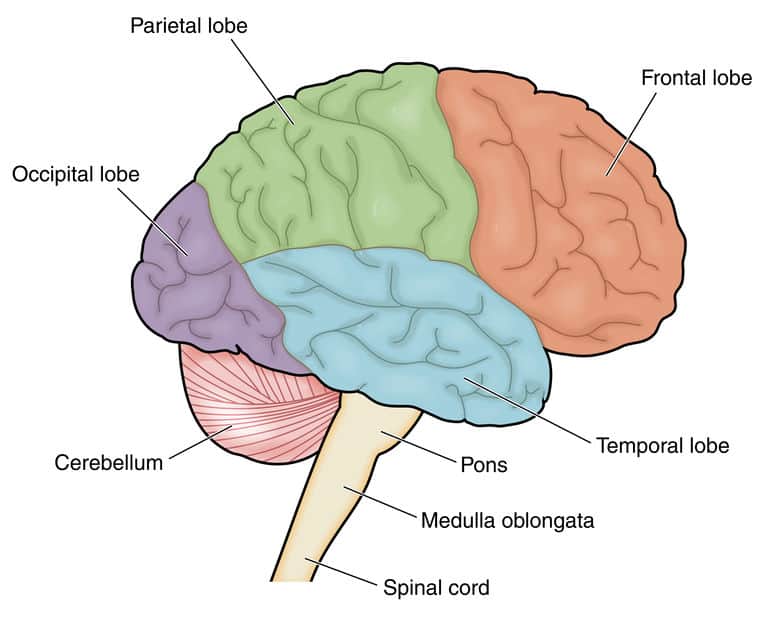
Other major forms include vascular dementia, dementia with Lewy bodies (abnormal aggregates of protein that develop inside nerve cells), and a group of diseases that contribute to frontotemporal dementia (degeneration of the frontal lobe of the brain).
The boundaries between different forms of dementia are often unclear, and mixed forms exist. The term mixed dementia used to describe a combination of two or more types of dementia.
4. What Is Alzheimer’s Disease?
The science of Alzheimer’s disease has come a long way since 1906, when a German neurologist and psychiatrist named Dr. Alois Alzheimer first described the key features of the disease. Dr. Alzheimer noticed abnormal deposits in the brain of a 51-year old woman who had dementia.
Alzheimer’s disease is defined as a neurodegenerative disorder of uncertain cause that primarily affects older adults. It is the most common cause of dementia.
One of the hallmarks of Alzheimer’s disease is the accumulation of amyloid plaques in the brain. Amyloid is a protein fragment that the body usually produces. In a healthy brain, these protein fragments are broken down and eliminated.
In Alzheimer’s disease, the amyloid fragments, particularly beta amyloid, accumulate to form hard, insoluble plaques.
Selective memory impairment is usually the earliest clinical manifestation of the disease.
The diagnosis of is based on the patient’s history and tests of memory, problem-solving, attention, and language. Standard medical workup is necessary to assess the general health of the patient and to exclude other causes for Computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET) may be performed to support the diagnosis.
Family history often plays a role. There is a higher risk of Alzheimer’s if a close family member has the disease. Having the ApoE4 genetic variant is one of the most significant risk factors for developing the disease (4).
Most cases of Alzheimer’s develop late in life, and most patients with the disease are 65 or older.
The risk of developing Alzheimer’s disease appears to be increased by many factors that affect the heart and blood vessels. These include high blood pressure, atherosclerotic heart disease, stroke, diabetes, and elevated cholesterol.
So, although there’s no definitive way to prevent the disease, not smoking, keeping blood pressure and cholesterol at healthy levels, regular exercise, maintaining a healthy weight, and eating healthy are all sensible measures.
Alzheimer’s disease is a progressive disorder, where dementia symptoms gradually worsen over several years. In its early stages, memory loss is mild, but with late-stage Alzheimer’s disease, individuals lose the ability to carry on a conversation and respond to their environment.
There is no cure available for Alzheimer’s disease. Although current treatments cannot stop the disease from progressing, they can temporarily slow the worsening of dementia symptoms and improve quality of life for those affected and their caregivers.
5. What Is Vascular Dementia?
Vascular dementia, also called vascular cognitive impairment (VCI), refers to any dementia that is primarily caused by cerebrovascular disease or impaired blood flow to the brain (5). It is the second most common cause of dementia, only exceeded by Alzheimer’s disease (6).
The symptoms of vascular dementia can vary widely, depending on the area of the brain affected by vascular injury. As in Alzheimer’s disease, memory loss is often pronounced.
Symptoms typical of cerebrovascular disease may often be present. Examples are difficulties with speech or walking and numbness or paralysis of one side of the face or body.
In many cases, a clinically diagnosed stroke appears to initiate the onset of symptoms. Hence the term poststroke dementia.
Multiple small strokes or vascular brain injuries may cause symptoms to occur more gradually.
The risk factors for vascular dementia are the same as those for stroke. Not smoking, keeping blood pressure, blood sugar, and cholesterol within normal limits, healthy eating, exercise, and limiting alcohol consumption are examples of measures that may reduce the risk of vascular dementia.
6. What Is Dementia with Lewy Bodies (DLB)?
Dementia with Lewy bodies (DLB) may account for 10-15 percent of all cases of dementia (7). Hence it is a common type of dementia.
The disease is associated with abnormal deposits of a protein called alpha-synuclein in the brain. These deposits, called Lewy bodies, affect chemicals in the brain leading to dementia characterized by problems with thinking, movement, behavior, and mood (8).
Lewy bodies are also found in the brains of patients with Parkinson’s disease.
In Parkinson’s disease, Lewy bodies are mainly found at the base of the brain, whereas in DLB, they tend to be found in the outer layers of the brain.
Diagnosing DLB may be challenging. Initially, the disease is often mistaken for Alzheimer’s disease. However, as the disease progresses, the patients usually develop symptoms typical of Parkinson’s disease.
Parkinson’s disease is usually associated with tremor, stooped posture, slow movement, and shuffling gait.
Furthermore, patients with Parkinson’s disease often develop dementia. Hence, the term Parkinson’s disease dementia.
Dementia with Lewy bodies (DLB) may account for 10-15 percent of all cases of dementia. The disease is associated with abnormal protein deposits in the brain called Lewy bodies. Patients with DLB usually also develop symptoms typical of Parkinson’s disease.
7. What Is Frontotemporal Dementia (FTD)?
Frontotemporal dementia (FTD) occurs when nerve cells in the frontal and temporal lobes of the brain die, leading to shrinking of these parts of the brain.
Formerly known as Pick’s disease, the name, and classification of FTD has been a topic of discussion for decades (9).
In fact, FTD is a group of heterogeneous neurodegenerative disorders characterized by noticeable changes in social behavior and personality or problems with language accompanied by degeneration of the frontal and/or temporal lobes (10).
FTD is a significant cause of dementia in younger people and is is most often diagnosed between the ages of 45 and 65.
The most common type of FTD is the behavioral variant, which is characterized by changes in personality and behavior.
Patients with the behavioral variant of FTD often lose their inhibitions and behave in socially inappropriate ways. They often lose interest and motivation and may show less sympathy or empathy. Their behavior may become repetitive, compulsive, and ritualized (11).
There may even be altered food preferences, such as carbohydrate cravings, particularly for sweet foods, and binge eating. Increased consumption of alcohol or tobacco may occur.
Primary progressive aphasia (PPA) is another clinical subtype of FTD. In PPA, the early symptoms are dominated by difficulties with language that progressively get worse. These are manifested by deficits in word-finding, word usage, word comprehension, or sentence construction (12).
Three variants of PPA have been described based on the type of language impairment: nonfluent, semantic, and logopenic (13).
As FTD progresses, brain damage bends to become more widespread. As a result, the symptoms are often similar to those of the later stages of Alzheimer’s disease.
FTD is highly heritable. An autosomal dominant pattern of inheritance is observed in the families of approximately 10 to 25 percent of patients (12). An additional 40 percent of patients report a family history of dementia or psychiatric conditions.
8. How Is the Cause of Dementia Identified?
The first step when evaluating patients with suspected dementia is determining whether it is present or not. Several disorders may cause symptoms that mimic dementia, and these have to be excluded. Hence, a thorough medical evaluation of the patient should be performed at the first visit.
Cognitive and behavioral testing is the first step to assess if dementia is present. These tests can be divided into three levels of rigor: screening tools such as the Mini Mental State Examination (MMSE), an extended mental status examination, and formal neuropsychological testing (3).
However, although these tests help to assess the quantity of impairment, a detailed patient history, including an interview with a spouse or another close relative, is of crucial importance.
Drug history is particularly important as many drugs can impair cognition.
All patients should be screened for depression. Cognitive impairment may sometimes be a key feature of depression. Furthermore, depression may often worsen cognitive impairment in patients with dementia.
Screening for B12 deficiency and hypothyroidism should be performed.
Neuroimaging with computed tomography (CT) or magnetic resonance (MR) may be helpful. In most cases, MRI is preferred over CT.
The use of positron emission tomography (PET) and single-photon emission computed tomography (SPECT) is an area of ongoing evaluation.
Symptoms of Parkinson disease may suggest dementia with Lewy bodies (DLB). Behavioral abnormalities and personality change in a relatively young patient may suggest the behavioral subtype of frontotemporal dementia (FTD). Language difficulties out of proportion to memory impairment suggest primary progressive aphasia (PPA).
9. What Conditions May Mimic Dementia?
Aging is associated with cognitive decline, usually consisting of mild changes in memory and the rate of information processing.
Most of us get more forgetful as we get older. We may sometimes struggle to remember names or put a signature to a face, and it may take a bit longer to find the right word. We may get distracted more easily or struggle to multi-task as well as we once did.
These changes are normal, but they can be a nuisance and at times, frustrating. Many people worry that these things are an early sign of dementia
However, these deficits do not tend to be rapidly progressive, nor do they affect daily function as they would if dementia was present.
Nutritional deficiencies, side-effects from medications, and emotional distress can all produce symptoms that can be mistaken as early signs of dementia. These may include memory impairment and behavioral changes.
Patients with depression often show signs of cognitive impairment that may mimic dementia. Memory loss and an inability to focus or concentrate may be pronounced. Working memory, fluency, and planning and problem-solving abilities may be impaired (14).
Some drugs may interfere with cognitive function and cause symptoms that may mimic dementia.
10. Can Drugs Cause Cognitive Impairment Mimicking Dementia?
Yes, they can.
Anticholinergic drugs, in particular, may negatively affect cognitive function. These include medications such as tolterodine, often used to treat urinary incontinence, some antidepressants, antipsychotics, some heart medications, antispasmodics, antivertigo medications, and antiparkinsonian medications (15).
A recent study even showed that exposure to several types of potent anticholinergic drugs is associated with an increased risk of dementia (16).
Benzodiazepines, a class of medications used to treat anxiety or insomnia, comprise another group that has been linked with cognitive difficulties.
The frequently used cholesterol-lowering statins have been suspected of creating memory difficulties and mental slowing in some people. However, there is still divided in opinion on this issue.
Cognitive changes associated with chemotherapeutic agents used to treat cancer have been documented. The condition is commonly called “chemo brain” or “chemo fog,” even though chemotherapy is unlikely the sole cause of these cognitive problems (17). The duration of chemo brain can vary from a few weeks to several years.
Pain killers, opioids, in particular, may negatively affect short-term memory.
11. What Is Mild Cognitive Impairment (MCI)?
Mild cognitive impairment (MCI) refers to cognitive impairment that is not severe enough to meet the criteria for dementia.
MCI is not an established diagnosis but refers to the transitional zone between normal aging and dementia (16). Although individuals with MCI have impaired cognitive function in specific domains, it is not severe enough to interfere with daily life.
However, it may be quite challenging to make the distinction between impairments that are normal for an adult and those that do represent MCI or dementia. What constitutes impairment in daily living is different for each individual (17).
MCI is relatively common. One study showed the following numbers for the prevalence of MCI (17):
- 6.7% for ages 60-64,
- 8.4% for 65-69,
- 10.1% for 70-74,
- 14.8% for 75-79,
- 25.2% for 80-84.
The risk of developing dementia in individuals with MCI older than 65 years followed for 2 years was 14.9%. Thus it appears that people with MCI have an increased risk of developing dementia compared to the average population.
Amnestic MCI is the most common subtype of MICI and refers to individuals with significantly impaired memory who do not meet the criteria for dementia (18). Otherwise, cognitive function is preserved, and activities of daily living are intact.
Amnestic MCI is often regarded as a precursor to Alzheimer disease (19)
Nonamnestic MCI may affect a single domain or multiple domains other than memory. Examples of such domains are executive functioning, language, or visual-spatial skills.

12. What Are the Risk Factors For Dementia?
Age is the strongest risk factor for dementia. The risk of Alzheimer disease increases rapidly after the age of 60 years. Overall, approximately 85 percent of dementia cases are in adults 75 years of age and older (20).
Genetic factors play an important role in Alzheimer’s disease. Parental history of dementia is associated with a twofold increase in the risk of dementia. Risk estimates gradually decline with advancing parental age at diagnosis of dementia (21).
APOE genotype status is a powerful risk factor for subsequent risk of dementia (4).
Cardiovascular risk factors are linked to increased risk of dementia. One large study showed that midlife diabetes, hypertension, and smoking are associated with an increased risk of dementia (22).
In the same study, total cholesterol level was not associated with an increased hazard of dementia. Other lipid fractions were tested in separate models and were not related to the risk of dementia.
Stroke is a risk factor for dementia. Approximately 10 percent of patients develop new-onset dementia after a first stroke, and up to one-third of patients develop dementia after recurrent stroke (23).
Mild cognitive impairment (MCI) may be considered a risk factor for dementia because it often progresses to dementia.
Diabetes is associated with an approximately 1.5- to 2-fold increase in the relative risk of cognitive decline and dementia later in life (23).
Studies indicate that midlife obesity increases the risk of dementia later in life (23).
Obstructive sleep apnea (OSA) has been associated with an increased risk for MCI and dementia. A very large pooled analysis showed that those with sleep-disordered breathing were 26 percent more likely to develop clinically relevant cognitive decline or dementia (24).
Low physical, mental, and social activity appears to be associated with an increased risk of dementia. Because these are all are modifiable factors, they may present options for decreasing the risk of cognitive decline and dementia.
Lower levels of education are associated with an increased risk of dementia (25).
Alcohol abuse is associated with increased risk of cognitive decline and dementia.
13. How Is Dementia Treated?
It is true for almost all of the diseases causing dementia that they cannot be cured.
Non-drug treatments of dementia mainly play a supportive role.
Cognitive rehabilitation aims to help patients in the early stages of dementia to maintain memory and cognitive function.
There is promising evidence that exercise programs may improve the ability to perform activities of daily life in people with dementia (26).
Other popular activities include music, singing, or art. It is vital that people with dementia stay as active as they can, physically, mentally, and socially. Taking part in meaningful activities is enjoyable and leads to increased confidence and self-esteem (27).
There are drugs available that may reduce the symptoms of dementia and possibly halt progression for a while. Cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine are frequently used for this purpose. These drugs appear to provide modest symptomatic benefit in some patients with dementia (28).
Memantine is an N-methyl-D-aspartate (NMDA) receptor antagonist. The drug which may protect brain cells and appears to have modest benefits in patients with moderate to severe Alzheimer’s disease. (28). There is little, if any, evidence that patients with milder disease derive benefit from the drug.
14. What Is the Prognosis of Patients With Dementia?
Dementia shortens life expectancy. Irrespective of the underlying cause, dementia is a progressive disorder.
The rate of progression for Alzheimer’s disease varies widely. The average life expectancy after the disease is diagnosed has been reported to be between 8 and 10 years but may range from 3 to 20 years (29). The degree of impairment at diagnosis will affect life expectancy.
The average life expectancy after a the disease is diagnosed has been reported to be between 8 and 10 years but may range from 3 to 20 years.
Older age of onset Alzheime’s symptoms is associated with a slower rate of decline compared with younger patients (30).
Like all other types of degenerative dementia, dementia with Lewy bodies (DLB) is a progressive disorder and associated with a shortened lifespan. Cognitive impairment and Parkinson symptoms both tend to worsen over time.
In general, the prognosis of DLB is similar to Alzheimer’s disease. However, in some patients, symptoms may progress faster and slower in others (31).
Early survival analyses showed median survival from diagnosis of frontotemporal dementia (FTD) to be 7–13 years in clinic cohorts (32). The behavioral type and primary progressive aphasia (PPA show comparable survival times. Survival is usually worse if concomitant motor neuron disease is present.
15. How Can dementia Be Prevented?
Seven modifiable risk factors have been associated with increased risk of Alzheimer’s disease (33).
- Diabetes
- Midlife hypertension
- Midlife obesity
- Depression
- Physical inactivity
- Smoking
- Cognitive inactivity or low educational attainment
It has been estimated that up to half of cases are potentially attributable to these modifiable risk factors.
Avoiding these factors may markedly reduce the risk of dementia.
Discover more from Doc's Opinion
Subscribe to get the latest posts sent to your email.
