Estimated reading time: 17 minutes
Syncope is the medical term used to describe the phenomenon of fainting or passing out.
Although syncope is common and frequently experienced by healthy people, it is often, quite wrongly indeed, considered a sign of frailty or illness.

Indeed, history shows that fainting spells occurring under the attention and scrutiny of the public may have harmed the reputation of some famous leaders.
Franklin Pierce, the 14th US president, passed out twice during battles in 1847. Subsequently, he was given the nickname “Fainting Frank” by his detractors.
In 1992, US President George H. Bush famously fainted after vomiting at a state dinner hosted by Japanese prime minister Kiichi Miyazawa.
Bush, who was 67 at the time, had played doubles tennis with the Emperor of Japan and his son that morning. He appeared to be in excellent health. However, during the dinner, Bush suddenly fell ill, leaned forward, then fell to his side, vomiting into the lap of his host, the Prime Minister.
The type of fainting Mr. Bush experienced is called vasovagal syncope and is characterized by slowing of the heartbeat and a fall in blood pressure.
Bush lost his re-election bid the following November. Many believe that his challenger, Bill Clinton, may have benefitted from the fainting incident. Clinton’s relative youth and vitality were crucial to his public image, and Bush’s public fainting probably served to reinforce the differences between the two men (1).
Scientific evidence suggests that at least nineteen percent of people will experience syncope at least once in their lifetime (2).
Fainting may occur at any age, but there is a significant increase in its frequency after 70 years of age (3).
The prognosis is determined by the underlying cause. The presence and severity of underlying heart disease tend to be decisive factors when addressing the seriousness of syncope.
+
1. What Is Syncope?
Syncope is a sudden loss of consciousness caused by a transient disruption of blood flow to the brain.
Typically, the inadequate blood supply to the brain is of a brief duration (8-10 seconds), and, in syncope, it is, by definition, spontaneously self-limited (4).
Syncope is associated with loss of postural tone. Postural tone is the steady contraction of muscles that are necessary to hold different parts of the skeleton in proper relation to the various and constantly changing attitudes and postures of the body (5).
Loss of postural tone leads to collapse, often resulting in injury due to a fall.
Recovery from syncope or true fainting is usually complete and fast, and episodes generally do not last more than a minute or two.
2. How Common Is Syncope?
Syncope is a common medical problem responsible for 3–5% of emergency department visits. Furthermore, there is a recurrence rate of approximately 35% (2).
In fact, syncope is responsible for 740,000 trips to the emergency department and a quarter of a million hospital admissions each year in the US alone (6).
The incidence of syncope shows a bimodal pattern. The first peak is in late adolescence and early adulthood, and the second peak is after 70 years of age.
There is a significant increase in the incidence of syncope after 70 years of age, with 5.7 episodes/1000 individuals per year between 60 and 69 years old and with 11.1 episodes/1000 individuals per year between 70 and 79 years of age. After 80 years, the annual incidence may reach 19.5 per 1000 individuals (2).
Syncope appears to be slightly more common among women than men (7).
3. What Is Presyncope?
Presyncope is the sensation that one is about to pass out. It is often described as a severe lightheaded feeling, often associated with unsteadiness or falling (8). The patient may feel that he is “nearly blacking out” or “nearly fainting.”
Most commonly, presyncope arises because the brain is temporarily not receiving adequate oxygen, usually because of diminished blood flow (9).
The causes of presyncope are generally the same as those of true syncope.
4. What Are the Most Common Causes of Syncope?
The following are the three most important initial steps in the evaluation of patients with suspected syncope:
- Comprehensive history
- Physical examination
- Electrocardiogram (ECG)
Additional diagnostic evaluation, if necessary, should be individualized based upon the suspected cause of syncope.
For the sake of simplicity, the causes of syncope can be grouped into three categories:
- Reflex syncope (also termed neurally mediated syncope)
- Orthostatic syncope
- Cardiac syncope
5. What Is Reflex Syncope (Neurally Mediated Syncope)?
Reflex syncope is the most common cause of fainting in younger individuals. It is also the cause of about half of cases in older individuals (4).
Other causes become more common with advancing age.
Reflex syncope comprises several related conditions in which neural reflexes that modify heart rate and blood pressure react inappropriately..
Typically, the mechanism behind reflex syncope involves both cardioinhibitory and vasodepressor features. These are induced by alterations in the responses of the autonomic nervous system (7).
The cardioinhibitory response is caused by an increased parasympathetic activation leading to a slowing of the heart rate (bradycardia).
The vasodepressor response is caused by decreased sympathetic activity leading to a drop in blood pressure (hypotension).
Typically, reflex syncope is short in duration (one to two minutes). However, full recovery may be delayed as the patient may feel fatigued for a while following the event.
Types of reflex syncope include vasovagal syncope, situational syncope, and carotid sinus syndrome.
Reflex syncope is usually considered a relatively benign phenomenon apart from the fact that sudden loss of consciousness may lead to an injury to the patient.
6. What Is Vasovagal Syncope?
Vasovagal syncope (also known as common faint) is the most frequent type of reflex syncope. Although common among the elderly, it is most often seen in young people.
Vasovagal syncope is typically associated with a precipitating factor, also known as a trigger.
Prolonged sitting or standing position, emotional stress, pain, heat, venous puncture, alcohol use, dehydration, and the use of certain drugs such as diuretics and vasodilators are typical triggers.
Before the patient loses consciousness, he or she often experience prodromal symptoms such as lightheadedness, a feeling of being hot or cold, sweating, palpitations, nausea, visual blurring, and diminution of hearing (10). Onlookers frequently report that the patient looked pale before and after he or she fainted.
Vasovagal syncope typically occurs in the sitting or standing position but not in the supine position. It typically has a short duration and usually does not last for more than one to two minutes. As in other types of reflex syncope, the patient often feels fatigued afterward.
Patients with a typical vasovagal syncope generally do not require further diagnostic evaluation.
While not directly responsible for increased mortality, repeated vasovagal syncope can hurt the daily lives of patients. This can take the form of both physical symptoms and injuries and psychological impact from living in fear of the next syncopal episode (11).

7. How Is Vasovagal Syncope Treated?
Recurrent vasovagal syncope affects the quality of life of many people.
As in other types of reflex syncope, the earliest priority is to inform the patient about the benign nature of their syncope. Educating and reassuring is a crucial first step in treatment (12).
Patients should be taught to maintain hydration, avoid hot conditions, and pay attention to their early symptoms and prodromes if present.
If there are specific triggers, efforts should target avoiding the trigger whenever possible.
Most Syncope Clinics recommend increasing the patient’s intake of dietary salt and water.
There is a multitude of physical treatments and maneuvers that can be helpful for patients with repeated vasovagal syncope.
Counterpressure maneuvers, such as tensing the arms with clenched fists, leg pumping, and leg-crossing, may abort a syncopal episode or at least delay it long enough that patients can assume the supine position (13).
There is no effective pharmacological treatment for most patients with recurrent vasovagal syncope. However, a small minority of patients with recurrent episodes can benefit from effective pharmacotherapy.
8. What Is Situational Syncope?
Situational syncope is essentially a reproducible vasovagal syncope with a known precipitant (14).
Micturition, defecation, swallowing, coughing, hunger, fear, and intense emotional stress are typical triggers for situational syncope.
The treatment involves avoidance of the precipitant when possible.
9. What Is Carotid Sinus Syndrome (CSS)?
Carotid sinus syndrome (CSS) is a disease of the autonomic nervous system presenting with syncope, especially in older males who often have cardiovascular disease. The etiology is unknown, and epidemiological data is limited (15).
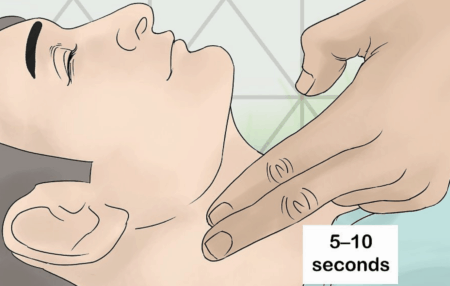
CSS is defined as syncope with a reproduction of symptoms during carotid sinus massage of 10s duration (16). A positive response is defined as heart rate pauses >3 seconds and a drop of systolic blood pressure >50 mmHg.
Patients with sinus carotid syndrome present with syncope with little or no prodrome.
For the sake of clarity, CSS is not the same as carotid sinus hypersensitivity (CSH).
CSH consists of the observation that carotid sinus massage results in a greater than expected fall in heart rate and a drop in blood pressure (17). This may happen in asymptomatic patients (e.g., patients without syncope).
Carotid sinus massage should be considered in all patients with syncope over the age of 40 years when the cause of syncope is not detected by the initial evaluation (18). Below the age of 40, CSS is sufficiently rare to allow omission of carotid sinus massage.
When performing carotid sinus massage, the patient is placed in the supine position with the neck extended to get proper access to the carotid artery. Pressure is then applied to one carotid sinus for 5 to 10 seconds.
Insertion of a cardiac pacemaker may be necessary for many patients with CSS.
10. What Is Orthostatic Syncope?
The term orthostasis is derived from Greek (orthos (upright) and histanai (to stand)) and basically means standing upright.
In medicine, orthostasis refers to the normal response of the sympathetic system to counteract a fall in blood pressure when a person assumes the upright position after lying down.
Orthostatic (postural) hypotension implies a pathological fall in blood pressure upon assuming an upright posture. It is a relatively common cause of syncope and near syncope.
When one stands up, gravity causes a shift of 500 to 800 mL of blood volume from the upper body to the lower body and the splanchnic circulation. This redistribution of blood decreases the return of blood to the right side of the heart, reducing the stroke volume of the ventricles which eventually can lead to a fall in arterial blood pressure (19)
Usually, due to several compensatory mechanisms, the body quickly counteracts the force of gravity and maintains stable blood pressure and blood flow. Hence, in most people, the drop in blood pressure is only transient and goes unnoticed (20).
However, if the body’s regulatory responses are disturbed or delayed, orthostatic hypotension can cause presyncope or syncope that may result in falls and injury, particularly in older adults.
The classical definition of orthostatic hypotension is a reduction of at least 20 mm Hg in systolic or of at least 10 mm Hg in diastolic blood pressure, measured 3 minutes after changing from a lying to a standing position (21).
Orthostatic hypotension is often considered as being either immediate or delayed (4).
Immediate orthostatic hypotension is fully resolved within 10 to 20 seconds after assuming the upright position.
However, delayed orthostatic hypotension occurs a few moments later, often one to several minutes after standing.
11. What Causes Orthostatic Hypotension?
Several factors may contribute to orthostatic hypotension.
Hypovolemia (a drop in the volume of blood) and dehydration (low fluid volume in the body) both increase the risk.
Hypovolemia and dehydration may be caused by inadequate fluid intake, bleeding, elevated blood sugar, diarrhea, vomiting. Furthermore, medications like thiazide diuretics (HCTZ) and loop diuretics (furosemide, bumetanide) may worsen the situation (22).
The risk of hypovolemia and dehydration increases in hot weather.
Medications that are used to treat elevated blood pressure, such as beta-blockers, calcium channel blockers, ACE inhibitors, nitrates, and angiotensin II blockers can induce orthostatic hypotension
Some medications for anxiety, depression, erectile dysfunction, and Parkinson’s disease may also promote orthostatic hypotension.
Alcohol consumption may cause orthostatic hypotension due to impaired vasoconstriction.
Anemia (low blood count) also increases the risk.
The risk of orthostatic hypotension increases with age. This may be due to impaired autonomic reflex response and the use of medications that promote low blood pressure.
Patients with diabetes and certain nervous system diseases are at increased risk of orthostatic hypotension due to a failure of autonomic reflex responses.
Patients with Parkinson’s disease often suffer from orthostatic hypotension.
12. How Is Orthostatic Hypotension Treated?
The goal of management is to raise the patient’s standing blood pressure and hence, the risk of syncope.
Treatment should always start with identifying and correcting the underlying cause or conditions that exacerbate the problem. Hence, ruling out hypovolemia, dehydration, and anemia is essential.
Increasing salt and fluid intake is usually recommended.
When orthostatic hypotension is caused or made worse by medications, treatment usually involves changing the dose or stopping drug treatment entirely.
For mild orthostatic hypotension, one of the most straightforward measures is to stand up slowly, in stages, from supine to seated to standing. Furthermore, sitting or lying down immediately after feeling lightheaded upon standing may help prevent injuries from falling.
Maintaining adequate hydration and avoiding overheating is vital for most patients.
Compression stockings and garments or abdominal binders may help reduce the pooling of blood in the legs and reduce the risks of orthostatic hypotension and syncope.
In some patients, treatment with drugs such as fludrocortisone, midodrine, and droxidopa (Northera) may be helpful.
Other medications, such as pyridostigmine (Regonol, Mestinon), nonsteroidal anti-inflammatory drugs (NSAIDs), and epoetin (Epogen, Procrit), are sometimes used.
Caffeine may improve orthostatic hypotension (23).
13. What Is Cardiac Syncope?
The term cardiac syncope is used to describe fainting caused by an underlying cardiovascular disease. Hence, it most often stems from a condition of the heart that prevents it from supplying enough nutrients and oxygen to the brain.
Cardiac syncope is estimated to be the underlying cause in 15% of syncopal events (24).
While the majority of syncopal events are innocuous, cardiac syncope is often indicative of a potentially fatal, underlying condition, carrying a one-year mortality rate of 30% (25). Hence, distinguishing cardiac syncope from other syncopal causes is highly important.
Mortality in these patients is mostly due to the severity of the underlying heart disease.
The underlying heart condition causing syncope may be a rhythm disturbance (arrhythmia), a structural problem, or a structural problem that predisposes a patient to a rhythm disturbance.
14. What Heart Rhythm Disturbances Can Cause Syncope?
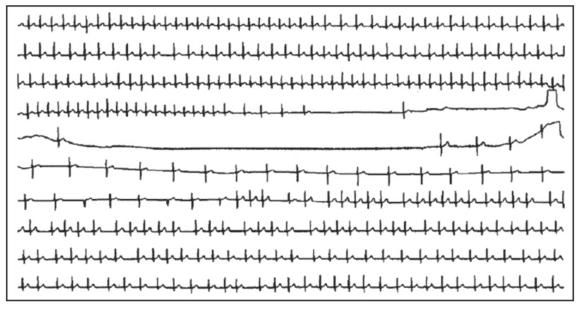
The term cardiac arrhythmia describes disorders of heart rhythm. All types of irregular or abnormal heart rhythm fall under this term. It may be an irregular rhythm or rapid or slow beating of the heart. The term tachycardia describes rapid beating of the heart, whereas the term bradycardia describes slow heart rate (25).
When arrhythmias cause syncope or presyncope, it is either due to bradycardia or tachycardia that does not allow adequate output of blood flow from the heart. As a result, blood pressure drops, preventing the brain from receiving adequate blood flow to maintain consciousness.
The most common cardiac arrhythmias causing syncope are AV-block, cardiac pauses (often due to sinus node disease), ventricular tachycardia, and supraventricular or atrial tachycardia.Patients with underlying heart disease (e.g., previous heart attack, valvular heart disease, hypertrophic cardiomyopathy, are at increased risk of cardiac syncope due to arrhythmia.
Individuals with congenital disorders affecting the electrical system of the heart, such as Brugada syndrome and long QT syndrome, are at increased risk of ventricular tachycardia leading to syncope and sometimes cardiac arrest.
15. How Is Cardiac Arrhythmia Causing Syncope Detected?
When history, physical examination, and ECG do not provide a definitive cause of syncope, further diagnostic testing may be warranted to exclude an underlying cardiac arrhythmia.
Frequently, the arrhythmia causing the syncope is no longer present when the patient undergoes medical examination
Ambulatory ECG monitoring devices are important tools for the diagnosis arrhythmia (26).
The holter monitor is a portable device that records and saves data. It is usually worn for one to three days and sometimes up to a week. At the same time, the patient keeps a diary of his/her symptoms. This may help to detect or exclude arrhythmia associated syncope or presyncope.
The implantable loop recorder (ILR) is implanted under the skin and can be used for much longer time periods (27).Special loop event recorders can save data for more extended periods, and direct transmission of signals may be possible through telephone (28).
Furthermore, different types of smartphone apps and watches are becoming frequently used to detect arrhythmia.
16. What Structural Heart Diseases Can Cause Syncope?
Structural cardiovascular diseases that may cause syncope include coronary artery disease, valvular heart disease (particularly aortic stenosis), hypertrophic cardiomyopathy, atrial myxoma, pulmonary embolus (blood clot in the lung due to venous thromboembolism), pulmonary hypertension, pericardial tamponade, and acute aortic dissection (4).
Echocardiography, a noninvasive examination of the heart, is an important tool to detect structural disorders of the heart. It provides images of the heart’s structure and function and helps to identify underlying heart diseases such as congenital or valvular heart disease and cardiomyopathy.
Examples of other cardiac imaging techniques that may be helpful are magnetic resonance imaging (MRI), computed tomography (CT), or nuclear medicine (NM) imaging with PET or SPECT.
17. What Disorders May Mimic Syncope?
It is important to understand that syncope is but one form of transient loss of consciousness.
Examples of conditions that may mimic syncope, but are not true syncope, are seizures, sleep disturbances (examples include narcolepsy and cataplexy), accidental falls, and some psychiatric conditions (4).
Metabolic disorders, including hypoglycemia (low blood sugar), hypoxia, and hyperventilation, may cause loss of consciousness that mimics syncope. Hypoglycemia primarily occurs in patients being treated for diabetes.
Seizures often mimic syncope. One distinguishing feature is that patients with seizures rarely have an abrupt recovery. Instead, the so-called postictal state following a seizure is characterized by a slow recovery.
18. What Questions Should Be Asked When Evaluating the Cause of a Transient Loss of Consciousness?
Obtaining a detailed medical history is the first step in determining whether a transient loss of consciousness is a true syncope or if there is another underlying cause.
The onset of syncope can provide important clues. Many patients with syncope have a brief period of symptoms (often called prodromal symptoms) of at least a few seconds before losing consciousness. Examples of such symptoms are nausea, sweating and feeling hot or cold.
Prodromal symptoms are typically associated with the vasovagal syncope, whereas a sudden onset of syncope without a prodrome is more common among patients with cardiac syncope.
The longer the period of time over which episodes have occurred (eg, many years versus very recent onset), and the earlier the onset of symptoms in terms of patient’s age (particularly when the first syncope occurs before age 35 years), the less likely that the cause of syncope is life-threatening (29)
Patients with benign causes of syncope such as vasovagal faint may have a history of multiple episodes over many years. However, a patient with multiple episodes occurring over a short period of time is more likely to be suffering from cardiac syncope, requiring urgent evaluation.
It is important to ask about the position of the patient when syncope occurred. Reflex syncope, including vasovagal syncope, almost always occurs when the patient is upright and not in the supine position.
Syncope caused by orthostatic hypotension usually occurs when the patient rises from a supine to erect posture.
Conversely, a syncope that occurs when the patient is supine is almost never a reflex syncope nor caused by orthostatic hypotension. Hence, it is more likely to be caused by cardiac arrhythmia.
True syncope is usually brief, and loss of consciousness usually does not last more than one to two minutes. A more prolonged loss of consciousness may indicate a seizure or a psychiatric disorder.
The Bottom Line
Syncope is a sudden loss of consciousness caused by a transient disruption of blood flow to the brain. Typically, the inadequate blood supply to the brain is of a brief duration (8-10 seconds).
Presyncope is the sensation that one is about to pass out.
The causes of syncope may be classified into three categories; reflex syncope, orthostatic syncope, and cardiac syncope.
Vasovagal syncope (also known as common faint) is the most frequent type of reflex syncope.
Orthostatic syncope is caused by a drop in blood pressure when a person assumes the upright position after lying down.
The term cardiac syncope is used to describe fainting caused by an underlying cardiovascular disease. While the majority of syncopal events are innocuous, cardiac syncope is often indicative of a potentially fatal, underlying condition.
The underlying heart condition causing syncope may be a rhythm disturbance (arrhythmia), a structural problem, or a structural problem that predisposes a patient to a rhythm disturbance.
Distinguishing cardiac syncope from other syncopal causes is highly important.
