Estimated reading time: 12 minutes
Cracks in the White Coat
The trust had always been silent.
It was the air in the room — unnoticed, unquestioned.
Doctors were the keepers of knowledge; patients were the grateful recipients.
That was how medicine had worked for centuries.
You obeyed, you recovered, you were grateful.
But outside the hospital walls, the world was beginning to roar.
It started as a tremor.
In the United States, the 1960s cracked open long-sealed hierarchies — civil rights marches, antiwar protests, and second-wave feminism. Authority figures were being questioned, mocked, sometimes torn down.
And Europe was erupting too.
In Paris, students filled the streets during the May ’68 uprisings, spray-painting the walls and shutting down universities.
Berlin, Rome — the same defiance, the same fury.
Even medical students joined in, demanding transparency, ethics, and a say in how they would be trained.
Medicine, long insulated by white coats and Latin, could not stay untouched.
The old certainty began to feel brittle.
The first cracks came quietly, in courtrooms.
In 1972, in Washington D.C., a young man named Jerry Canterbury was left partially paralyzed after spinal surgery. His surgeon hadn’t told him paralysis was a risk.
The judges ruled that he should have been told — and for the first time, they said what patients had never been allowed to say out loud:
You have the right to know, and the right to choose.
Across the Atlantic, change came more slowly.
In Sidaway v. Board of Governors (1985), Britain’s highest court still sided with the old way. It said doctors could decide which risks to mention, as long as other doctors would have done the same.
It kept the power with the physician — for a while.
Then, in Montgomery v. Lanarkshire (2015), that changed.
The court ruled that doctors must tell patients about any risks a reasonable person would want to know.
It ended the idea of “doctor knows best” and made consent a duty, not a kindness.
For centuries, doctors had relied on therapeutic privilege — the belief that too much information might harm the patient, so it was kinder to withhold it.
But now the law said otherwise.
Informed consent was no longer a gesture of kindness. It was a duty.
The white coat could no longer shield a decision from scrutiny.
And something subtle shifted.
Trust was no longer automatic.
It had to be earned.
Then the scandals surfaced — one after another, like bruises coming up to the skin.
The Tuskegee syphilis study, exposed in 1972, showed how hundreds of Black men had been denied treatment for decades without their consent.
Thalidomide had been sold as safe to pregnant women, leaving thousands of babies with severe birth defects and shattering public trust across Europe.
At Willowbrook, disabled children were deliberately infected with hepatitis in the name of research.
Each story said the same thing: obedience had allowed harm to hide.
And each one left a deeper scar: the realization that the system itself could not be blindly trusted to protect the vulnerable.
Hospitals began posting “Patient Bills of Rights” on their walls.
Bioethics committees formed to review decisions once made behind closed doors.
Medical schools started teaching not only anatomy and pharmacology, but also communication, consent, and ethics.
Medicine was still paternalistic, but something had shifted.
Patients were no longer content to be silent.
They wanted — and now had — a voice.
What began as quiet autonomy was, underneath, something else:
Doubt.
And soon, that doubt would no longer whisper.
It would shout.
In the shadow of a new epidemic, patients would move from the waiting room to the war room — and the pedestal would crack open.
The Revolt
By the early 1980s, the cracks in medicine’s hierarchy had widened.
Then came the virus that blew the doors off.
It arrived quietly at first — strange infections, rare cancers, young men dying of diseases that didn’t belong to them.
In hospital wards, the beds filled.
Patients wasted away while doctors stood at the foot of their beds, powerless — and, sometimes, distant.
They were young. Mostly gay. Mostly men.
And many were treated not as patients, but as pariahs.
Research was slow.
Funding hesitant.
Compassion scarce.
Families were shunned.
Coffins were sealed.
And so they fought back.
In New York, they chained themselves to the doors of the FDA.
They interrupted scientific conferences, occupied pharmaceutical offices, and stormed the headquarters of the National Institutes of Health.
They didn’t wear white coats.
They wore black T-shirts that said:
Silence = Death.
They weren’t asking for permission anymore.
They were seizing power.
They called themselves ACT UP, and they changed medicine more than many medical breakthroughs ever did.
They forced the FDA to speed drug approvals and open “parallel track” access to experimental treatments.
They won seats for patients on advisory boards and clinical trial committees.
They rewrote how studies were designed, which endpoints mattered, and who got to speak at the table.
Some were dying as they marched — IV poles rattling behind them — but they marched anyway.
They had no time left for hierarchy.
And the revolt was not confined to America.
In London, the Terrence Higgins Trust fought for dignity, treatment, and the right to be seen.
In Paris, AIDES challenged stigma with public protests and legal campaigns.
In Amsterdam, the Schorer Foundation launched outspoken education drives, forcing the government to act.
Across Europe, patients were no longer content to plead.
They demanded power — and for the first time, they began to get it.
Then came the Internet.
Suddenly, medical knowledge was no longer locked behind library doors and paywalls.
PubMed, WebMD, patient forums, and early blogs — for the first time in history, patients could read the same studies as their physicians.
They began arriving at consultations armed with printouts, acronyms, and questions once whispered only in conference rooms.
Doctors were no longer the sole keepers of knowledge.
The white coat had lost its monopoly.
By the late 1990s, the doctor–patient relationship had been rewired.
Consent was no longer a signature on a form; it was a conversation.
Patients expected not just to be told what would happen, but to choose what would happen.
This was not yet antagonism — not quite.
But the old obedience was gone.
And with it, the aura of unassailable certainty began to fade.
For a fleeting moment, the old hierarchy seemed to soften —
patients bringing knowledge, doctors offering partnership.
But then came the pandemic — and the fragile trust that held the system together cracked wide open.
The Trust Fracture
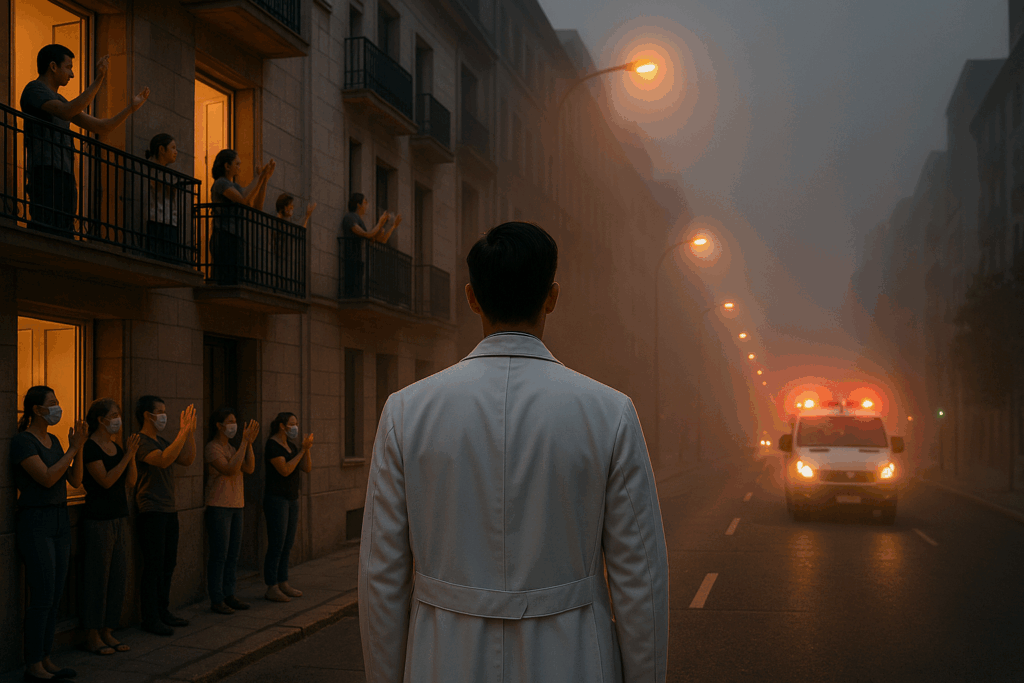
For a brief moment, it felt as if medicine had gone back in time.
In the spring of 2020, as sirens wailed through empty city streets, people leaned from balconies to applaud doctors. Hospital workers were hailed as heroes. The white coat was back on its pedestal.
But it didn’t last.
At first, the old hierarchy flickered to life.
People waited for clear orders.
They obeyed curfews, masked without debate, deferred to experts on television.
The public craved certainty, and doctors tried to provide it.
But the science was still forming — and science, by nature, shifts.
To scientists, changing guidance was the rhythm of discovery; to the public, it looked like chaos — or betrayal.
The old contract of obedience had depended on the illusion of certainty.
COVID tore that illusion to pieces.
And when the vaccines arrived, they should have been medicine’s redemption —
instead, they became symbols in a cultural war.
Social media amplified everything: the triumphs, the fears, the fabrications.
Disinformation spread faster than any virus, and often farther than the truth.
Doctors were attacked online, doxxed, or forced to become influencers just to stay heard.
Expertise no longer commanded authority.
It had to compete for it.
Something deeper had shifted.
Science was no longer seen as a method — a way of testing, correcting, and converging on truth.
It was seen as a performance, a moving target, maybe even a trick.
COVID hadn’t just shaken trust in doctors —
it had cracked the deeper trust that science itself could be relied on.
Something more fundamental than hierarchy had broken:
trust in the machinery of science.
When the smoke cleared, the pedestal was gone.
What remained was not trust, but noise —
and a new kind of medicine where authority had to be earned from scratch.
This is the world in which medicine works today.

Doctors did this to themselves. They overwhelmingly and sheepishly went along and went against all that virology had taught them. Then they put it on display of dancing nurses and dancing doctors and Talking Heads on all the TV channels telling us with certainty what was going to happen to those that didn’t get the jab. You go back to the AIDS crisis, but you never mentioned that it was the distrust and the mismanagement and possibly illegal activity of Dr. Fauci where they hung him and effigy in the 80s. I was there I remember… For giving AZT and saying wait for vaccine, which to this day has never come, he killed millions And he killed millions more with Covid protocols of Remdisivir and ventilation and and there wasn’t an army of doctors protesting still to this day, doctors who did protest at the time are still being harangued by their medical associations…
so you have brought this upon yourselves doctors, you have caused this distrust by not standing up in mass and saying enough! this is not medicine. This is propaganda and greed… For us on the outside I’d rather take the risk of my fellow citizens and my own research, which is equal to what you learn and sometimes better because… I’m not that good at memorization so I have to store all my information carefully away, and I don’t have a God complex… That makes me different than most doctors
I think you’re right — doctors do carry part of the blame. Some of the trust that was lost wasn’t taken from us; we gave it away, through overconfidence or silence. But abandoning science entirely can’t be the answer. It’s still the only tool we have to separate truth from noise — and our task now is to make it worthy of trust again.
Brilliant, having lived & worked through the last 50+ years as a Physician being the patriarch was comfortable but medical knowledge has expanded at such a rate that teamwork (patient plus medic) has to be the norm. Feel that AI will replace most current medical contact (accurate diagnosis including mental health with accurate synapse chemical monitoring ?in the breath)
Follow-up by empathetic robotic surgeon or physician happy days!
Beautifully put — the old patriarchal role may have been comfortable, but it’s no longer possible or even desirable. Medicine has become too vast for any one mind to command, and partnership with patients is the only sustainable path forward.
I agree that AI will transform diagnostics — maybe even aspects of mental health — but I suspect what will matter most is what can’t be automated: empathy, trust, and human presence. The science may become faster, but the listening will still take time.
Another brilliant thought provoking article. I have been involved in emergency medicine for almost 40 years and have seen many of the changes you mention in your article. Having been apart of some of the epidemics and pandemics you mention. I do agree with the core message – that we need to work together, the patient needs to a part of an integral multi disciplinary approach/team. The “trust” that needs to be rebuilt is a challenge, I have also believed in science and that science will guide us thorough the quagmire of all the various studies and how to dissect them to best care for our patients. As you say evidence is not an opinion, we can have an opinion about the evidence, but it does not change what the evidence has stated/shown/proven.
The challenge is real with respect to patient care, what I have learnt is that when the opportunity arises to build a “relationship” built on trust and informed dialogue, real progress can be made with patient care in a respectful space. Yes, as Andre says in his reply – Doctors did have a god complex, as did other fields of care, Emergency medicine was no different, but there has been real change and real effort by many health care practitioners, who abode by a Patients Rights Charter, and follow good clinical guidelines, to throw the baby out with the bath water would be dangerous.
If we can be anything during this process of change – lets just be kind – and that would apply to all within the treatment paradigm.
Mike
Thank you, Mike — that means a lot, especially coming from someone who has stood on the frontlines for so long. You’ve captured exactly what I hoped to convey: that trust won’t return through authority, but through relationships — built slowly, through dialogue, humility, and care.
I share your belief that science will guide us through the noise, but only if we anchor it in humanity. Evidence may light the path, but trust is what allows patients to walk it with us. And as you say, kindness matters — perhaps more than ever.
Thank for an interesting piece. I do think that nutritional guidance over the past 50 years has accelerated the loss of confidence. Folks go low-fat high- carb because they’re told to, get obese and diabetic and wonder what the hell.
Thank you — and I agree this has played a role. Decades of shifting and sometimes misguided nutritional advice have left many people feeling misled, even betrayed. When guidance backfires, trust erodes — and rebuilding it means being far more honest about uncertainty, nuance, and how evidence evolves.
I think the problem with doctors is that there is still too much of “Me Doctor (MD) and you not”) attitude. MD’s don’t really want to have a back and forth discussion with patients. They want to process the patient as quickly as possible and then usher them out the door. NEXT!
Additionally, in my experience, most MD’s fail to keep up with research and advances in their speciality field. Too many rely on info they learned in medical school 20, 30 or 40 years ago. Their response to problems is pure rote and they lack curiosity.
This is why I champion AI doctors and will be happy when most MD’s are replaced by AI.
I get the appealJojo — AI won’t interrupt you, won’t have an ego, and won’t be running late from the last patient. But it also won’t notice if you’re scared, or if something about your story doesn’t quite fit the algorithm. Doctors can be stubborn, yes — but that stubbornness is often just the weight of responsibility. AI will give you answers. It just won’t care if they’re the wrong ones.
“or if something about your story doesn’t quite fit the algorithm”
——
I think you have this backwards. For the vast majority of MD’s, it is the humans who practice rote medicine and are unable to see outside the algorithm that runs their brains. This is why the rate of misdiagnosis/unable to diagnose runs so high among human MD’s.
Here’s an article/system you should find interesting:
The Path to Medical Superintelligence
by Dominic King & Harsha Nori
June 30, 2025
The Microsoft AI team shares research that demonstrates how AI can sequentially investigate and solve medicine’s most complex diagnostic challenges—cases that expert physicians struggle to answer.
Benchmarked against real-world case records published each week in the New England Journal of Medicine, we show that the Microsoft AI Diagnostic Orchestrator (MAI-DxO) correctly diagnoses up to 85% of NEJM case proceedings, A RATE MORE THAN FOUR TIMES HIGHER THAN A GROUP OF EXPERIENCED PHYSICIANS. MAI-DxO also gets to the correct diagnosis more cost-effectively than physicians.
—
https://microsoft.ai/new/the-path-to-medical-superintelligence/
That’s a thoughtful point. You’re right — rote medicine, where doctors follow algorithms without deeper reasoning, is part of the problem. AI systems like MAI-DxO may well raise the bar for diagnostic accuracy, and I think they’ll increasingly become partners in care.
But even the best diagnosis — whether from a human or an AI — still depends on trust. If evidence is perceived as opinion, or if recommendations feel imposed rather than shared, the conversation between medicine and patients breaks down. That, to me, is the real challenge: not just getting the answer right, but making sure it can still be believed.
Speaking of medical mistrust, I am sure that you will find this story very interesting and instructive.
—-
I created my own AI medical team. It changed the way doctors treat my cancer
AI didn’t replace my human specialists, but it supercharged my decision-making
By Steve Brown
Sept. 10, 2025
When I turned 60, I knew something wasn’t right. I lost weight. I felt drained. I had no appetite. I had a gut feeling — literally, abdominal discomfort — and a sense that something serious was going on beneath the surface. So I asked my doctors to test everything.
Full body scans. Colonoscopy. Endoscopy. Cardiac function tests. Every lab test I could get approved.
The gastroenterologist removed a couple of polyps but said nothing was wrong other than mild gastritis. The cardiologist suggested that maybe I was stressed or depressed. Then the Palisades fire destroyed our Los Angeles house, and my wife and I were displaced to Palm Desert, Calif. A few weeks later, I was suddenly in severe pain that lasted a weekend. Nothing stayed down.
By Monday morning, I was a patient in the emergency room in a new health system. These doctors — strangers completely unfamiliar with my history — saw my case with fresh eyes. Within days, they found what everyone else had missed: an aggressive form of blood cancer in my bone marrow related to multiple myeloma. They had caught it early, but it was already starting to affect not only my bone marrow but also my kidneys, gut, and heart if we did not stop it fast.
Lying in a hospital bed for nine days, I couldn’t stop thinking. Why couldn’t my first doctors find anything? Would AI have caught my disease sooner?
…
https://www.statnews.com/2025/09/10/ai-cancer-treatment-custom-doctors-response/
Also suggest looking at his website:
http://www.curewise.com
In the US, insurance-doctor contracts and the medical group policies (group profit driven) limit those “conversations”. Medicine is a business under multiple “department of efficiency” bean counters.