Estimated reading time: 7 minutes
🎧 Available in audio
You can listen to this article, The Myth of the Routine Procedure, narrated in full. Whether you’re walking, driving, or just prefer to hear it aloud, click play below.
He was on the list for what we called a routine coronary angiography—possible PCI if needed.
Mid-sixties. Retired electrician. Lived alone. The kind of man who apologized when the nurse missed his vein.
“Bad veins, sorry,” he said, as if it were his fault.
The morning had gone smoothly. Five patients down, two to go. The rhythm of competence had settled in—steady, predictable, almost comforting. Someone joked about the coffee machine. Another mentioned the football match that night. The monitors blinked in their familiar green pulse, the hum of the room as normal as breathing.
The Question
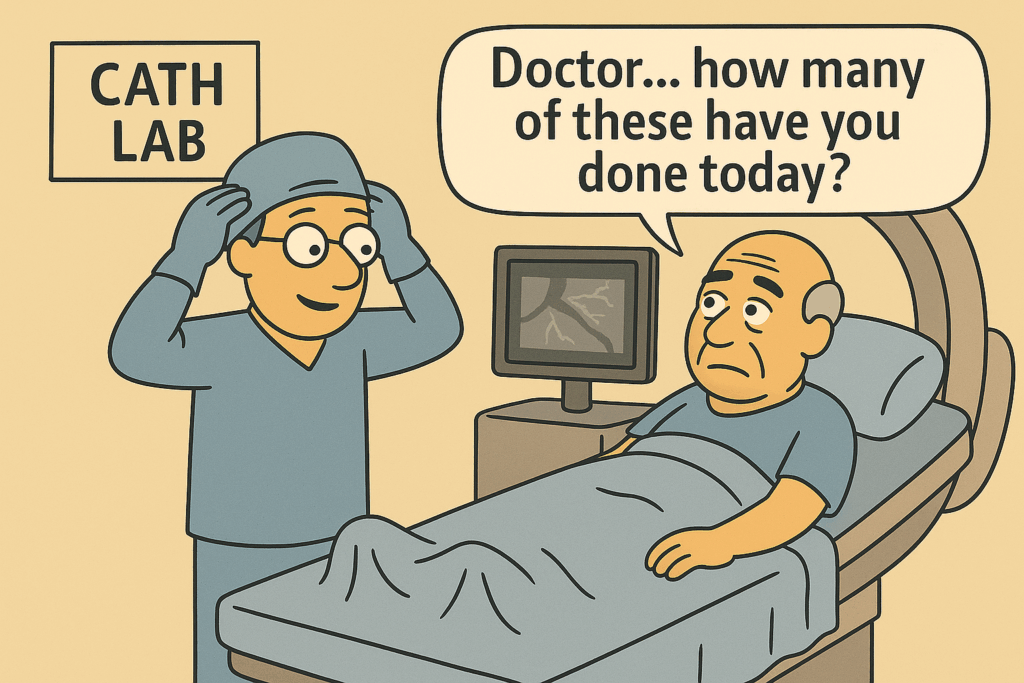
When I walked into the lab, he was already on the table—monitors in place, IV lines taped, the sterile drapes still folded at his side. He turned his head slightly as I came closer, eyes calm but searching. I rested a hand on his shoulder and said his name.
That’s when he spoke—softly, almost apologetically.
“Doctor… how many of these have you done today?”
I almost answered with a number. It would have been easy. But his voice carried something under the words—a small tremor, a need.
He wasn’t asking about experience. He was asking if I was still there. If I could still see him—not the artery, not the lesion, not the case—but the person.
The Drape
Before I could answer, the nurse laid the sterile drape across his chest and adjusted the radiation shield, lowering it into place like a quiet curtain between us.
And just like that, he disappeared behind it.
The moment always feels the same.
A quiet shift in gravity.
The sound of cloth settling.
The transformation of a human being into a field of operation.
The drape went up; the world divided.
He could no longer see us. He could no longer move his arms.
He could no longer reach for anyone.
He was awake, aware, and completely in our hands.
Two Worlds
No one teaches that moment in training. We learn about access, anticoagulation, contrast load—but not about consequence. Not about the transfer of power that happens when the drape rises and someone’s world narrows to sound and imagination.
I looked over the top of the sterile barrier—the faint rise and fall of his chest, the monitor beeping steadily.
“Ready when you are,” the nurse said.
For him, the word ready meant surrender.
For me, it meant control.
The two are not the same.
The Room
From the console, the room looked calm.
Fluoroscopy screen glowing.
Music low but steady.
Team moving in rhythm—the choreography of competence.
Someone adjusted the pressure line. Someone checked the stent sizes. Someone made a joke about lunch.
It wasn’t disrespect. It was survival.
When you live inches from catastrophe, you learn to keep the fear out of your hands.
To us, it was precision.
To him, it was captivity.
He heard every sound—every click of the injector, every whisper of the guidewire. The hum of the X-ray arm overhead. The casual conversation about weekend plans that floated above him like weather he couldn’t escape.
We forget that patients hear us. Not just our words, but our tone—the calm or the distance in our voices.
We speak in code: “smooth case,” “tight lesion,” “good flow.” But for them, those words are the soundtrack to uncertainty.
Two realities unfold in the same room:
One clinical. One existential.
We fix an artery. They face their own mortality.
Familiarity and Distance
Experience teaches us control.
It keeps our hands steady when the vessel dissects, when pressure drops, when there is no reflow.
We need that steadiness—it’s what saves lives.
But experience also breeds distance.
Risk turns into numbers: one in a hundred, one in a thousand.
Numbers are how we survive the arithmetic of danger.
But patients don’t live in statistics.
For them, risk isn’t a probability.
It’s a face, a thought, a prayer whispered beneath sedation.
It’s Will I wake up?
It’s Will I still be me?
That’s the asymmetry of procedural medicine: one act, two experiences.
We manage physiology.
They surrender control.
Over time, familiarity helps us function—but it also dulls sensitivity.
Our technique sharpens. Our attention narrows.
And sometimes, our awareness of meaning thins out like air at altitude.
Under the Drape
Under the drape, the world turns into sound and light.
I’ve watched it countless times—the ceiling too close, the lights too bright, the patient’s eyes darting beneath half-closed lids.
Every sound lands differently there: the soft hiss of oxygen, the click of metal, the quiet language of a team speaking around, not to, the person who can’t move. Every silence feels longer than it should.
You can almost sense the moment trust becomes physical—the surrender of control, the stillness that says, I’m counting on you now.
It isn’t written in the consent form.
It’s wordless, weightless, and absolute.
And it isn’t limited to the cath lab.
The same quiet surrender happens in endoscopy rooms, during colonoscopies and cystoscopies, in orthopedic theatres and ophthalmic suites—anywhere people remain conscious while strangers work inside their bodies.
The setting changes; the feeling does not.
It’s the same equation of trust and exposure, of stillness offered in exchange for safety.
The Procedure
Half an hour into the case, the lesion yielded.
Wire through. Balloon inflated.
The screen filled with the shimmer of contrast, that fleeting moment when flow returns and the heart’s geometry looks whole again.
“Good flow,” someone said.
“Looks perfect,” said another.
And it did.
Angiographically perfect.
But there’s always something invisible that lingers—something that can’t be measured in TIMI grades or frame counts. The unspoken understanding that, for the person on the table, this is the closest they’ve ever been to not coming back.
When the stent is deployed, the heart becomes an image—fixed, simplified, clean. But the human story doesn’t fit on a monitor.
The Return
The procedure ended without incident. The nurse cleaned the puncture site, removed the drape, began to roll him toward recovery. For the first time in forty minutes, he could see the faces around him.
He blinked under the light, dazed, searching.
Then his eyes found mine.
It’s always a small thing, that moment of return.
The look that asks, wordlessly, Am I safe?
Did it go well?
Was I ever really alone?
I nodded.
“You did great,” I said quietly.
And for a second, the question he’d asked before the drape went up echoed back.
How many today?
I thought of the others—their names, faces, the sameness of the routine that hides how singular each moment really is.
I couldn’t remember them all.
But I remembered him.
The Meaning of Routine
We call it a routine procedure.
To us, that means skill, safety, predictability.
To the patient, it sounds like something ordinary.
And nothing about lying half-sedated on a metal table while strangers thread instruments into your heart is ordinary.
Routine is a safety term.
It must never become a state of mind.
Because every time the drape goes up, someone disappears behind it—and it’s our job to remember they’re still there.
Technical skill keeps people alive.
Awareness keeps medicine human.
When the day ends and the gloves are off, the memory that lingers isn’t the stent or the angiogram—it’s the eyes that met mine when the world came back into view.
He’d asked how many I’d done that day.
Now I think about how many he did.
Just one.
And for him, it was everything.
Author’s Note
This isn’t about cath labs or wires or stents.
It’s about trust—the quiet kind that isn’t written in charts or measured in outcomes.
It’s given in silence, when someone lets you hold their heart for a moment and expects you to give it back.
And that is never, ever routine

Poetic and insightful, thanks
bob