Estimated reading time: 11 minutes
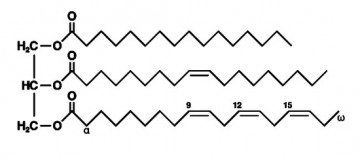
Triglycerides are important organic compounds. Most of the fat we consume in our diet is triglyceride and so is most of the fat we store in our body.
Fatty acids contained in triglycerides are an essential source of energy for human cells.
![]()
Triglyceride concentration can be measured in blood and may provide valuable information about metabolism and general health. High levels may reflect underlying metabolic disorders and evidence shows that high blood triglycerides are associated with increased risk of heart disease (1,2,3).
However, association only means that there is a correlation between two or more variables. In this case, the higher the blood triglycerides, the higher the risk of developing heart disease.
Hence, discovering an association between variables does not prove a causative relationship. Here, a correlation between triglyceride levels and the risk of heart disease does not prove that triglycerides cause heart disease. Nor does it prove that lowering them will prevent disease.
Interestingly, when it comes to assessing the risk of cardiovascular disease, triglycerides have always played second fiddle to cholesterol.
As a result, dietary advice for people with heart disease usually aims at lowering blood cholesterol, particularly LDL-cholesterol. Targeting LDL- cholesterol has become common practice.
Therefore, replacing saturated fat with polyunsaturated and monounsaturated fats, and increasing the intake of food products rich in fiber and complex carbohydrates such as whole grains, is usually recommended.
Interestingly, it may be tricky to address triglycerides at the same time as LDL cholesterol. The reason is that a diet that lowers LDL cholesterol may raise triglycerides and vice versa. For example, low-fat diets may lower LDL cholesterol but are less effective in lowering triglycerides compared to low-carbohydrate diets (4).
Another reason why main stream medicine has tended to ignore triglycerides is that the pharmaceutical industry has shown limited interest in developing drugs that influence triglycerides. However, this may have changed recently with the publication of the highly important REDUCE-IT trial (5).
Triglyceride-Rich Lipoproteins
High blood levels of triglycerides are most often associated with high levels of the two most important triglyceride-rich lipoproteins; chylomicrons and very low density lipoproten (VLDL).
The main role of these lipoproteins is to transport triglycerides and other types of lipids, such as cholesterol, in the circulation.
Chylomicrons are formed in the intestine after a meal. They contain triglycerides and small amounts of cholesterol.
Chylomicrons are subsequently broken down by an enzyme called lipoprotein lipase into free fatty acids that are utilized for energy production by the heart and skeletal muscles or stored in fat (adipose) tissue.
The chylomicron remnants are then removed from the circulation by liver cells.
VLDL is produced by liver cells. It transports both triglycerides and cholesterol. Once in the circulation, VLDL is broken down by lipoprotein lipase in capillary beds, releasing triglycerides for energy utilization by cells or storage in adipose tissue.
The composition of VLDL changes when triglycerides have been released. VLDL then becomes becomes intermediate-density lipoprotein (IDL). Later, when the amount of cholesterol increases, IDL becomes low-density lipoprotein (LDL).
Triglyceride-Rich Lipoproteins Are Associated With Inflammation and Atherosclerosis
Triglyceride rich lipoproteins are associated with inflammation and increased atherosclerosis (6).
High levels of chylomicrons increase the risk of acute pancreatitis, an inflammation of the pancreas. Chylomicron and VLDL remnants increase inflammation of the endothelium (the innermost layer of the artery).
Chylomicron remnants and VLDL remnants have been shown to rapidly penetrate the arterial wall and promote atherosclerosis (7).
Recent data suggests that VLDL cholesterol or remnant cholesterol is a stronger promoter of atherosclerosis than LDL cholesterol (8).
Definition of Normal and High Levels of Triglycerides
Blood levels of triglycerides are stratified according to population data and their associated risk of coronary artery disease.
In the USA, triglycerides are measured in mg/dL but in Australia, Canada, and most European countries they are measured in mmol/L.
To convert from mg/dL to mmol/L, divide by 88.5
Here is how triglyceride levels are looked at in terms of cardiovascular risk:
Normal: <150 mg/dL (1.7 mmol/L)
Borderline high: 150 to 199 mg/dL (1.7 to 2.2 mmol/L)
High: 200 to 499 mg/dL (2.3 to 5.6 mmol/L)
Very high: ≥500 mg/dL (≥5.7 mmol/L)
The term hypertriglyceridemia is used to describe high blood levels of triglycerides.
Hypertriglyceridemia is a relatively common disorder. In the United States, 33 percent of adults have triglyceride levels above 150 mg/dl (1.7 mmol/L) and 18 percent have levels above 200 mg/dl (2.3 mmol/L)(9).
Fasting and Non-Fasting Levels of Triglycerides
Following a fatty meal, blood levels of triglycerides will rise. Hence, raised blood triglycerides following a meal (postprandial hypertriglyceridemia) are caused by chylomicrons produced in the intestine.
Chylomicrons disappear from the circulation soon after the triglycerides have been delivered to the tissues.
Moderate fasting hypertriglyceridemia is usually due to increased VLDL production by the liver. This is often a result of excessive carbohydrate intake.
Triglycerides may also become elevated with obesity, physical inactivity, smoking, diseases such as diabetes and renal failure, drugs such as estrogen, tamoxifen and corticosteroids, and genetic disorders (familial hypertriglyceridemia, familial combined hyperlipidemia, and familial dysbetalipoproteinemia).
There are several types of familial hypertriglyceridemia. These disorders are associated with increased risk of coronary artery disease (10) which appears independent of cholesterol levels (11).
Serum triglyceride values above 1000 mg/dL (11 mmol/L) are rare (less than 1/5000 individuals). The serum in these patients is opalescent due to an increase in VLDL or milky due to elevated chylomicrons.
Triglycerides and Cardiovascular Disease
Despite evidence that chylomicron and VLDL remnants promote atherosclerosis, the importance of lowering triglycerides has so far not been considered a priority for patients with coronary heart disease.
However, several conditions associated with high triglycerides, such as insulin resistance, a preponderance of small LDL particles, and low HDL- cholesterol, may play an important role in the development of atherosclerosis.
Reduced activity of lipoprotein lipase, which is common in insulin resistance, may slow the clearance of triglyceride-rich lipoproteins from the circulation.
VLDL remnants may enter the vessel wall or be converted to small LDL particles. Small LDL particles tend to circulate for a longer duration where they become susceptible to oxidation, glycation, and glyco-oxidation leading to increased risk of atherosclerosis.
Small dense LDL particles appear more strongly associated with the risk of cardiovascular events than larger particles (12,13).
In the so-called SCRIP trial, high triglyceride levels were associated small, dense particles in 90 percent of subjects whereas lower triglyceride levels were associated with larger buoyant particles in 90 percent of subjects (14).
Recent genetic studies have addressed the relationship between triglyceride-rich lipoproteins and the risk of cardiovascular events. The results of one of these studies imply that the elevated cholesterol content of triglyceride-rich lipoprotein particles may cause coronary heart disease (15).
Another study found that a genetic mutation associated with low blood levels of triglycerides was associated with less risk of cardiovascular disease (16).
These studies strongly support the hypothesis that high blood levels of triglycerides may increase the risk of cardiovascular disease and that low levels may be protective.

The REDUCE-IT Trial – A Landmark Cardiovascular Study
The results of the REDUCE-IT trial were recently published in the New England Journal of Medicine and The Journal of the American College of Cardiology) (5,17).
The study randomized 8,179 statin-treated patients with triglycerides ≥135 and <500 mg/dL and LDL-cholesterol >40 and ≤100 mg/dL , and a history of atherosclerosis (71% patients) or diabetes (29% patients) to icosapent ethyl 4g/day or placebo.
Icosapent ethyl is a highly purified and stable EPA ethyl ester that has been shown to lower triglyceride levels.
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are the two most common long chain n-3 polyunsaturated fatty acids (PUFAs) in fish oil. Both are omega-3 fatty acids.
The primary cardiovascular outcome of cardiovascular death, nonfatal myocardial infarction, stroke, coronary revascularization, or unstable angina, for icosapent ethyl vs. placebo, was 17.2% vs. 22.0%. The absolute risk reduction of 4.8% is highly significant.
Triglyceride levels were lowered at one year by 39.0 mg/dl vs. 4.5 mg/dl on on icosapent ethyl vs. placebo. LDL cholesterol was lowered by 2 mg/dl vs. 7 mg/dl.
The rate of cardiovascular death was 9.6% vs 12.4 % on icosapent ethyl vs. placebo which is statistically significant. All-cause mortality was 6.7% vs. 7.6%, which is not statistically significant.
The risk of atrial fibrillation/flutter was 5.3% vs 3.9% and the risk of serious adverse bleeding was 2.7% vs. 2.1% on icosapent ethyl vs. placebo
Why Is the REDUCE-IT Trial so Important?
The large number of important ischemic events averted with icosapent ethyl, including a significant reduction in fatal and nonfatal stroke (28%), cardiac arrest (48%), sudden death (31%), and cardiovascular death (20%), is indicative of a very favorable risk- benefit profile
Although several mechanisms may explain the efficacy of the drug it has to be assumed that the lowering of blood triglycerides is the most important.
The study results are in stark contrast to cardiovascular outcome studies with other agents that lower triglyceride levels and with low-dose omega-3 fatty acid mixtures, where cardiovascular outcome benefit has not been consistently observed in statin-treated patients (17).
The distinction of the cardiovascular benefits observed in REDUCE-IT from the lack of cardiovascular benefits observed in statin-treated populations with add-on omega-3 fatty acid mixtures may likely be due to the high EPA levels.
EPA has unique lipid and lipoprotein, anti-inflammatory, anti-platelet, anti-thrombotic, and cellular modifying effects.
REDUCE-IT is the first trial to show that lowering triglycerides without affecting LDL-cholesterol significantly improves clinical outcome in high risk patients.
With the rapidly increasing prevalence of central obesity and metabolic syndrome , targeting triglycerides me even become more important in the near future.
Whether targeting triglycerides by dietary measures will improve cardiac outcome remains to be proven.
However, it would be naive to believe that dietary measures that tend to lower triglycerides are less important than those intended to lower LDL-cholesterol.
The Management of High Triglycerides
Non-Pharmacological Therapy
Lifestyle modification is the first-line therapy for people with elevated triglycerides.
Many individuals with high triglycerides have insulin resistance and metabolic syndrome. In these cases, hypertriglyceridemia is often associated with visceral obesity low levels of HDL cholesterol, high blood pressure and type 2 diabetes.

For these patients, weight loss, regular physical exercise, and avoidance of added sugars (18) are all important. Other risk factors such as smoking and high blood pressure should also be addressed (19).
Fatty acids used by the liver to produce VLDL are derived mainly from two sources.
Firstly, during conditions such as obesity, diabetes, and insulin resistance, there is increased fatty acid flux from adipose tissue to the liver. Secondly, there is an increased de novo synthesis of fatty acids in the liver mainly from carbohydrates.
For this reason, in mild to moderate hypertriglyceridemia, losing weight and reducing carbohydrate intake (especially high glycemic index foods and high fructose foods) can lower VLDL and triglycerides.
Dietary fat is not a significant source of liver triglyceride (20), and high fat diets usually don’t raise fasting triglycerides.
The situation may be different in more severe hypertriglyceridemia (above 500 to 1000 mg/dL (5.6 to 11.3 mmol/L)), where the clearance of chylomicrons becomes very slow. Under these circumstances, it is crucial to reduce dietary fat intake to lower triglycerides.
It is necessary for patients with severe hypertriglyceridemia to avoid alcohol abuse as it can cause substantial increases in triglyceride levels and cause acute pancreatitis.
Pharmacological Therapy
Several drugs are used for the management of hypertriglyceridemia.
Although statins are not very effective for lowering triglycerides per se, they are often used to reduce the risk of cardiovascular events in patients with hypertriglyceridemia.
One of the most commonly used drug to lower triglycerides is gemfibrozil (21).
Gemfibrozil belongs to a group of drugs called fibrates which lower triglycerides by increasing the synthesis of lipoprotein lipase which increases the clearance of triglycerides.
Fibrate therapy with either fenofibrate or gemfibrozil can reduce triglyceride levels by 20 to 50 percent. In severe hypertriglyceridemia, gemfibrozil may lower triglycerides as much as 70 percent (22).
In the Helsinki Heart Study, a clinical benefit of gemfibrozil therapy was found in the group with a triglyceride level >201 mg/dL (2.3 mmol/L) and an LDL-C/HDL-C ratio >5.0 (23).
The VA-HIT trial assessed the efficacy of gemfibrozil in patients with low HDL cholesterol, relatively low LDL cholesterol, and mild to moderate hypertriglyceridemia (24). Gemfibrozil raised HDL cholesterol by 6 percent, lowered triglycerides by 31 percent, but had no significant effect on LDL cholesterol. At five years, there was an absolute risk reduction of 4.4 percent with gemfibrozil.
In the ACCORD Lipid trial, fenofibrate improved outcomes in type 2 diabetes in a subset of patients with elevated triglyceride levels and low HDL cholesterol (25).
Nicotinic acid at doses of 1500 to 2000 mg daily can reduce triglyceride levels by 15 to 25 percent (26). However, studies supporting a clinical efficacy of nicotinic acid are lacking. There is data suggesting worsening of glycemic control when nicotinic acid is administered to patients with type 2 diabetes (27).
The AIM-HIGH trial studied the addition of nicotinic acid to statin therapy in patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of less than 70 mg/dL (1.81 mmol/L)(28).
There was no incremental clinical benefit from the addition of nicotinic acid during a 36-month follow-up period, despite significant improvements in HDL cholesterol and triglyceride levels.
Intake of fish oil (29) can lower blood triglycerides by as much as 50 percent (30). Relatively high doses of omega-3 fatty acids (EPA + DHA) are needed to achieve this effect (up to 3-4 g/day).
Lovasa (Omecor) and icosapent ethyl (Vascepa) are commercial preparations of omega-3 fatty acids that can lower blood triglycerides by as much as 45 percent (31,32).
Having metabolic syndrome and triglycerides so high that LDL couldn’t even be measured, I cant remember exactly, 685 I think, the doc told me go vegan and put me on a stain. The statin and diet lowered my other points to below thresholds but the triglycerides stayed above 300.
Then I had a statin related muscle injury and come to find out I can’t take those. So repatha was next. It tanked all my numbers, incredibly low, total cholesterol was only 91, yet triglycerides were still 256! Then the insurance said no repatha so off all meds again.
All the numbers went right back up even on vegan. I got very frustrated and decided to take matters into my own hands and went low carb, zero sugar, and added a few lean meats and cheeses back in. I am not low carb high fat by any means, still all veggies. However, zero fruit.
My latest blood test after two months on this diet, triglycerides 140. Slightly elevated nonhdl and ldl but total cholesterol very good with zero meds. Added side note. Over all this time I have lost about 40 pounds, but even at the 30 lost point eating vegan with whole grains, fruits etc my numbers were still sky high.
The advice doctors are giving that include grains and fruits, any insulin spikers in insulin resistant patients like metabolic syndrome type is wrong. The realization is coming around to that I believe.
Interesante articulo, importante para tener en cuenta. Gracias por compartirlo